If you’ve seen the latest ads for the video game Call of Duty, they are almost guaranteed to have left an impression.
First-person view, blasting through doors, dodging bullets, jumping off buildings with Taylor Kitsch as your right-hand man. The graphics are, simply put, amazing. Thanks to the tremendous improvements in computer graphics cards, video games today provide more realistic visuals through advances like higher resolution, more frames per second, greater diversity in color, and finer gradations of shading. Gamers demanded greater realism and faster action; developers responded. But it’s not just gamers who are reaping the benefits of superior gaming: the same technological advances are now making real improvements to how doctors treat cancer patients.
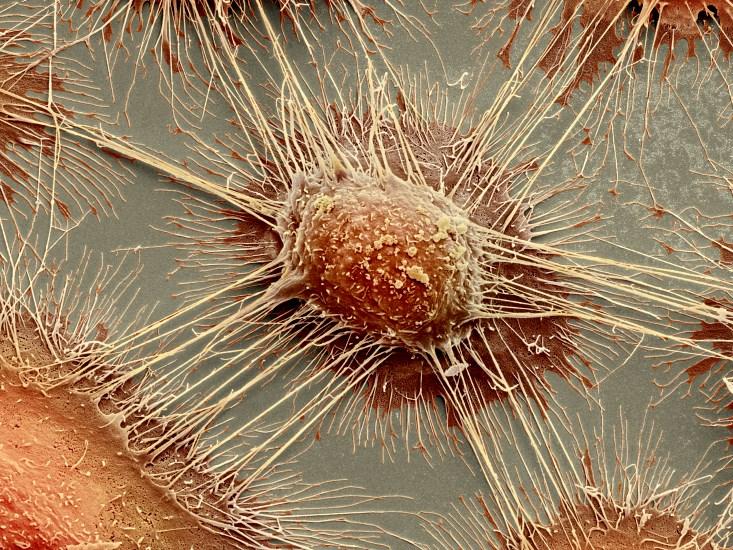
Radiotherapy—zapping cancer cells with a dose high-energy photons or charged particles, like electrons or protons—is one of the key tools in fighting cancer, but it’s particularly tricky business. Radiation oncologists must deliver the beam to the mass of cancer cells while avoiding the normal cells surrounding the tumor site; determining the right dose, location, and duration is a complex calculation. Targeting one abnormal section in an organ like the prostate, which contains billions of cells, requires extreme precision. How much radiation is the right amount? How will it affect neighboring cells? The variation between the patients’ anatomies makes the calculation for each individual that much harder. And perhaps worst of all, tumors can change substantially over relatively short times. “The human body is a dynamic system, changing from day to day. A tumor can shrink. Or the whole thing can move, being pushed by the rectum, bladder,” says Steve Jiang, a professor of medical physics at UT Southwestern*. “A static treatment strategy cannot be optimal. Yet, adapting our treatment to the patient’s dynamic anatomy requires a tremendous amount of computational power.”
Currently radiology departments run simulations of radiotherapy treatments “offline,” or after the patient has gone home, and they often require three days to complete. First a patient comes in for their radiation appointment. A CT scan of the tumor gives radiation oncologists an idea of where the tumor is on that day, at that moment. Then doctors run a simulation on software that calculates the path of the beam on its way to the tumor site. It then prescribes a radiation treatment, zeroing in on the spot where the tumor was at the time of the scan.
But a lot can happen in 70 hours between scan and treatment. The tumor can move or change by itself or due to the movement of the body around it. “If there is a tumor on a patient’s neck that shrinks from say, the size of an apple to the size of a ping pong ball [between one visit and the next], then you have to do the treatment redesign offline,” says Jiang. “It will take a few days. But for each patient under the machine, we only have about 20 minutes. And patients cannot wait for hours, days.”
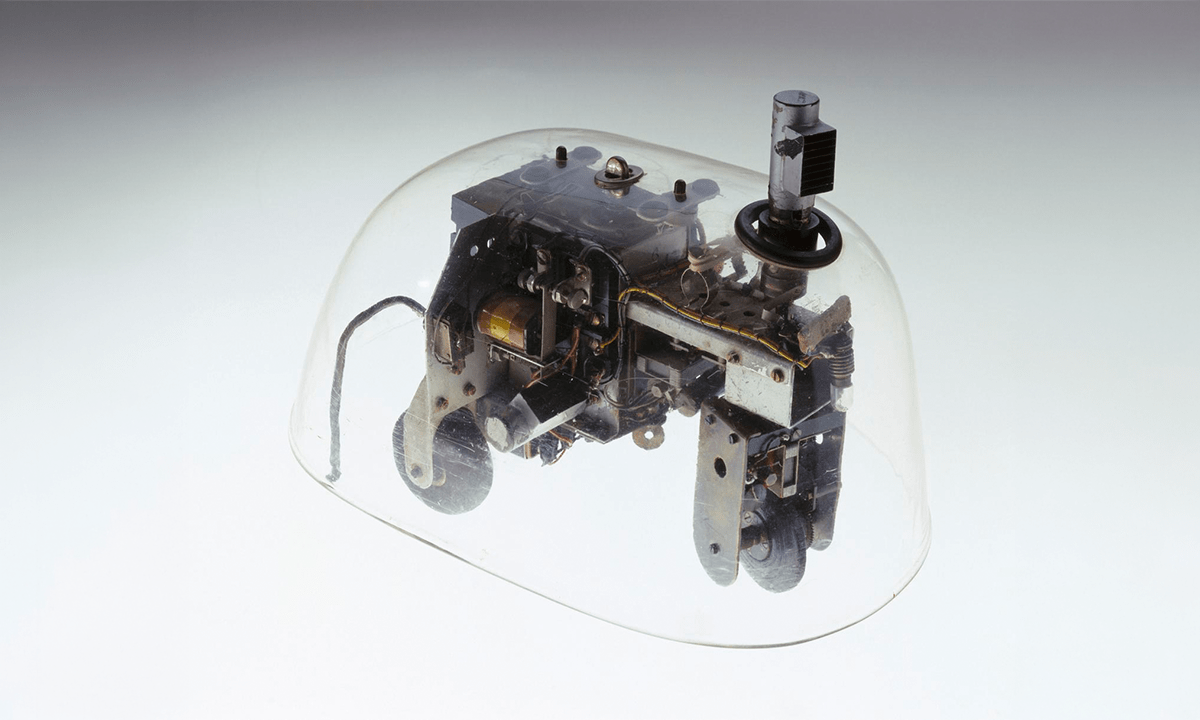
Fortunately a new tool has emerged to practically eliminate this delay—the same tool that started to dramatically speed up video-game graphics around 15 years ago: the GPU (graphics processing unit) in computer graphics cards. Before that period, the CPU—central processing unit, a computer’s general-purpose brain—handled all the computations necessary for any programs, games to word processors, to run in a computer. For the mass of computations involved in fast, colorful, detailed graphics, though, the CPU fell short. So manufacturers started relying on specific cards dedicated to the task of handling graphics. Kayvon Fatahalian, a computer scientist at Carnegie Mellon, says the difference between handling graphics on GPUs and CPUs is like the difference between a 10,000-lane highway with maximum speeds of 30 miles per hour and a two-laner with max speeds of 70. “GPUs are designed to do millions of things at a time very quickly, like executing computations made for games and synthesizing the pictures we put on screen. They simply were meant to do something else. CPUs are primarily designed to do a very small number of things [even more] quickly,” says Fatahalian.
Part of this distinction comes from the different structures of the chips. “GPUs have more than 2,000 microprocessors. In comparison, CPUs can have 4 cores, or 8 cores,” says Jiang. And since GPUs are manufactured by the million for computers and video-game consoles, the “price for each card is quite low.”
But the massive improvement to graphics hardware was not enough by itself to make graphics cards useful for cancer radiotherapy. One problem with older GPUs was the proprietary language they used was not easy to decipher for those who weren’t elite programmers. “Because cards were designed for video games, you had to program software by pretending [it] was a video game,” says Jiang. “But around 2007, the major vendor, Nvidia, came up with new language called CUDA, which made programming [the cards] much easier.”
So around 2009, Jiang started ordering cards from Nvidia, and he and his team began developing algorithms for radiotherapy computations. After a few years of research and experimentation with the graphics cards, Jiang’s updated model of radiation simulation—called “online adaptive radiotherapy”—required only tenths of seconds instead of 70 hours. With simulations that quick, doctors would be able to calculate the right dose for the right spot right before administering radiation for cancer patients.
“GPU processors are so efficient for these types of computations that it makes sense that they’re the right platforms,” says Fatahalian. “Essentially, any computation that’s related to image processing is a computation that works pretty well on these [graphic cards].”
Bradley Erickson, a professor of radiology at the Mayo Clinic in Minnesota, also jumped to use the graphics cards once he and his team worked out the software. “In CT scanners, we developed an algorithm that reduces [graininess] in images. On multi-core, Intel-type CPUs, the denoising takes around 40 to 50 minutes. But once we got the math right to adapt it to run on GPUs, we got it to work in about a minute. That means radiologists don’t have to wait close to an hour to get image results.”
Jiang believes in only a year or two, patients getting treated for cancer in hospitals will start seeing his online adaptive radiotherapy in place. His team has developed an algorithm, which runs on graphic cards, that quickly resolves how each energized particle travels inside the patient’s body, where the radiation particles deflect, where they stop, and where energy finally deposits, which determines beam’s biological effects. The simulation then determines the best treatment plan for that moment—not for days in the future. A secure tablet or phone application will provide a visual map of the recommended treatment plan. Once the doctor approves the plan, the patient will be treated right then.
“Gamers, they drive research and development. They’re a much stronger [economic] force than federal funding,” says Jiang. “And now we think with online adaptive radiotherapy, we can save patient lives, for sure.”
*Correction: The article originally listed Steve Jiang’s affiliation as UC San Diego. He actually moved from UC to UT Southwestern in 2013.
Yvonne Bang is Nautilus’ assistant editor/video production manager.