Just like every new drug the oncologists at Memorial Sloan-Kettering Cancer Center tested against bladder cancer in the last 20 years, this one didn’t seem to be doing any good. Forty-four people in the study were given everolimus in a last-ditch attempt to slow down or stop their advanced cancer. When the researchers analyzed the data, they could see that the drug wasn’t slowing or stopping tumor growth. Everolimus seemed to be another bust.
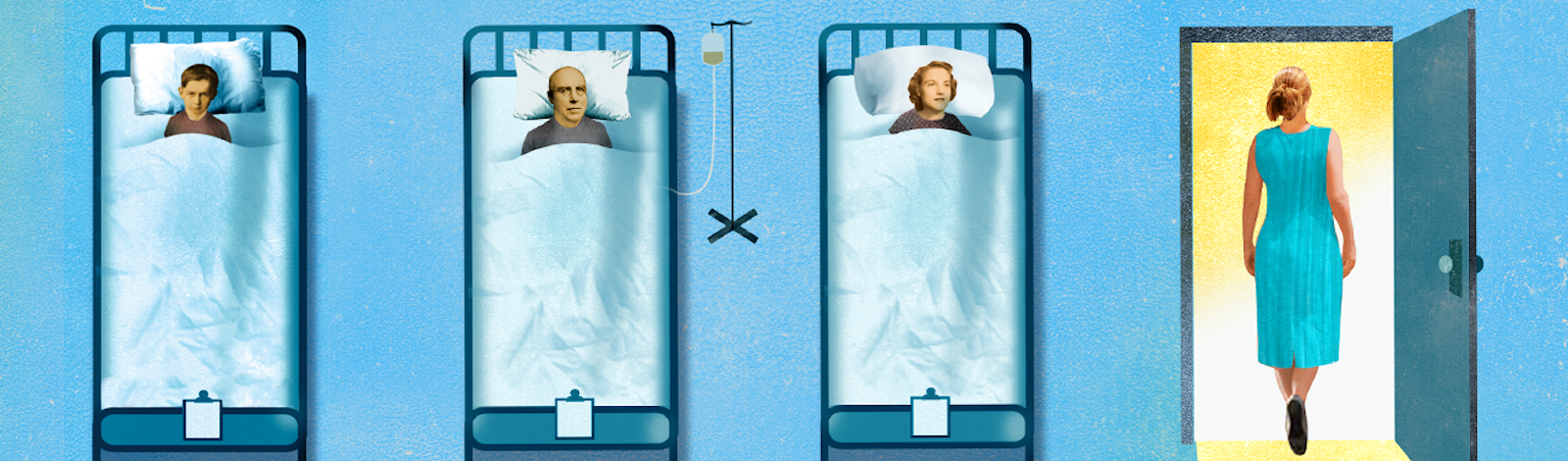
Then there was patient number 45. She joined the trial with advanced metastatic cancer. Tumors had invaded deep into her abdomen, clouding her CT scan with solid grey blotches. She was 73 years old. None of the standard bladder cancer drugs were working for her anymore; she had “failed treatment,” in the dismal lingo of oncologists. She enrolled in the study only because she happened to be a patient at Sloan-Kettering in January 2010. In April 2010, her cancer was gone.
This sort of happy surprise is not unheard of in drug studies. Bodies are fluky, each with its own idiosyncratic combination of genetic blueprints and environmental inputs. So sometimes a patient will be cured by a drug that is useless for everyone else. In the past, these spectacular reactions were written off as outlier responses that defied explanation—medical mysteries. Doctors just shrugged their shoulders and thanked their lucky stars that even though the study tanked, they did manage to help one person.
But this time was different. Clinical oncologist David Solit, director of developmental therapeutics at Sloan-Kettering, saw a new opportunity to explain what happened by sequencing the whole genome of the woman’s cancer. Just five years ago, decoding and analyzing all 3 billion bases of the DNA from a tumor would’ve been absurdly time-consuming and expensive. Now the sequencing takes as little as a few days.
Poring over the outlier patient’s genetic code, Solit pinpointed two mutations that made her tumor sensitive to this drug. He found that one of her mutations shows up in about 8 to 10 percent of other bladder cancer patients, meaning that they too might be helped by everolimus. His success has inspired a whole set of programs to study “exceptional responders”: those rare cancer patients who do well while nobody else does.
Cancer is a personal disease, Solit explains. Each tumor constitutes its own world of defective genes and proteins. By studying the genetic quirks of exceptional responders, physicians can systematically identify weaknesses in cancer subtypes and blast them with drugs that target their unique vulnerabilities. “It’s a testament to how much has been learned about the genome in the past 30 years,” Solit says. “We’ve always wanted to find out why some individuals respond so well. Now we have the capacity. It’s going to really change the way we treat patients.”
Unlikely cases have an eminent history in medicine. The modern science of the mind owes a lot to the freakish accident suffered by Phineas Gage, a 19th century railroad construction foreman whose job involved packing down explosive powder with a three-and-a-half-foot-long iron tamping rod. On Sept. 13, 1848, the powder exploded in his face, blasting the rod up through his chin and out the back of his head. Against all odds, he survived. But his personality was transformed. The formerly shrewd and patient Gage became obnoxious and unreliable.
An observant doctor named John Martyn Harlow who cared for Gage proposed that his personality change was due to the destruction of the frontal lobe of the left side of the brain. Gage’s unlikely transformation revealed a universal truth about brains, that particular parts—the frontal lobes—are required for self-control. The strange case of Phineas Gage is still mentioned in neuroscience textbooks.
Rare events can also lead to new cures. As the story goes, English physician Edward Jenner’s observations of an 18th century milkmaid who caught cowpox and thereby became immune to smallpox paved the way for the first vaccines. New ideas for curing HIV are emerging from the famously unlucky lucky case of the “Berlin patient.” Timothy Ray Brown, who was HIV positive, developed blood cancer leukemia in 2006. His chemotherapy and radiation treatments wiped out the cells of his immune system, where the virus is believed to hide. He then got a bone marrow transplant from one of those rare people with a gene mutation that makes them resistant to HIV. Today, Brown still has no sign of HIV in his body, and his case has inspired a study to genetically engineer HIV-positive patients’ cells to resist the virus.
“We’ve always wanted to find out why some individuals respond so well. Now we have the capacity. It’s going to really change the way we treat patients.”
In the past, cancer researchers weren’t able to capitalize on their unexpected outlier successes. Not enough was known about the biology of cancer, and the right tools hadn’t been invented. “Even if someone had a complete remission, you had no way to figure out why,” says James Doroshow, director of the Division of Cancer Treatment and Diagnosis of the National Cancer Institute (NCI). That changed in the 2000s, when it became possible to analyze the genetics of cancer tumors for clues.
The first major success came with studies of the drug gefitinib in non-small-cell lung cancer (the most common kind). Gefitinib helped less than 20 percent of the people who took it, but a few outliers had dramatic, rapid recoveries. In 2004, two Harvard groups found that the responders had mutations in the epidermal growth factor receptor (EGFR) gene. EGFR is one of many genes that regulates how cells grow and when they die, and the mutation basically forced it to pump out two or three times as much growth signal as it should, fueling the cancer. Gefitinib dialed down the signal. A clinical trial later proved that the drug keeps tumors at bay for more than nine months in people with certain EGFR mutations.
More insights gleaned from extraordinary responders soon followed. One melanoma patient in a study of 22 people taking sorafenib saw his tumor shrink quickly, a response due to a mutation in the gene KIT, which regulates cell growth, division and survival. People with certain kinds of melanoma, such as the type that grows on mucous membranes, now routinely get tested for this mutation. The drug helps about 40 percent of those with the mutation—an impressive advance in a cancer that once had no effective treatment.
In these studies, investigators had to make educated guesses about where in the genome to look for the culprit mutations. It was the keys-under-the-lamppost phenomenon: They could only examine genes they already suspected were involved in the cancer. But as the speed and efficiency of DNA sequencing skyrocketed, and its price plummeted, it started to look reasonable to sequence the whole tumor genome to cast the widest possible net. By 2010, when the bladder cancer patient (who doesn’t want her name made public) had such a wonderful response to everolimus, the technology was ripe to analyze her entire tumor.
The outlier patient had already gone through several rounds of treatment, including surgery at Memorial Sloan-Kettering. That was another stroke of luck because it allowed Solit’s group to acquire samples of her tissue to be sequenced. Cancers typically start with mutations that cause cells to divide too much, ignoring normal stop signals and evading quality controls that repair or prevent errors in DNA reproduction. “Cancer is a disease of mutations,” says Solit.
The outlier patient’s cancer had accumulated 17,136 mutations, of which 140 seemed most suspect, because they appeared in “coding” regions of the genome, the segments that include instructions on how to build the proteins that do the work in a cell. Out of those 140, two looked particularly menacing to Solit. In a gene called TSC1, just two of its 8,600 DNA base-pairs were missing, but the error would cause the gene to make a defective version of the protein it was supposed to create. In the gene NF2, an error meant a protein would be built only halfway, unable to do its job.
Solit could now see how these mutations were affected by everolimus, a drug typically used to suppress the immune system after organ transplants, and to combat advanced kidney cancer. Everolimus shuts down one crucial link in a chain of interacting proteins called the mTOR pathway that fuels cell growth, division, and survival. The drug inhibits the cells of the immune system from dividing, which they must do in order to attack foreign tissue, and protects transplanted organs. Likewise, it slows down the uncontrolled cell division that happens in cancer. The kicker was that both of the woman’s mutations, NF2 and TSC1, affect the mTOR system. “It’s not surprising, in retrospect, that our patient responded really well to this specific drug,” Solit says. “She had the mutation that activated the pathway the drug targets.”
Solit’s team analyzed 13 more people from the trial and found different TSC1 mutations in three other people, including two whose tumor shrank a little in response to the drug. (Nobody else had NF2 mutations, which is probably why she alone responded dramatically.) Meanwhile, eight of nine people whose tumors grew during the study did not have the mutation.
Doroshow of the National Cancer Institute says Solit’s work “turned on the lightbulb.” It showed how the analysis of exceptional responders could be made systematic. Inspired by his example, the NCI is now trawling through its own archives, revisiting outlier responses among the roughly 10,000 patients who enrolled in NCI-sponsored clinical trials during the last decade. Picture the long rows of crates in the government warehouse at the end of Raiders of the Lost Ark: There’s treasure in there somewhere, if only someone would look. “We ought to study these people more, since we have the means now,” says Barbara Conley, the associate director of the cancer diagnosis program at NCI, who leads the project.
In the few months since the project began, Conley’s team have already found about 100 exceptional responders. The next steps are to find out if their tumors were biopsied, if that tissue sample is still sitting in a freezer somewhere, and whether it’s in good enough shape to be sequenced. Starting next year, the group will start inviting any scientist who is doing a clinical trial to submit new cases.
The NCI project will include whole-genome sequencing (provided they have adequate tissue samples) and repeated reads of the whole “exome”—the 1 percent of human DNA that is translated into exons, the sequences that are used as templates for protein construction. The reason to do both, explains Conley, is that cancer cells, even within a single tumor, often have a hodgepodge of mutations. Re-doing whole exome sequencing dozens of times captures most of the significant genetic variation in one tumor, and it’s more practical than trying to sequence the whole genome over and over. Finally, RNA expression will also be analyzed. Evaluating RNA, an intermediary between DNA and proteins, provides a measure of which genes are switched on and how much protein they’re producing.
Picture the long rows of crates in the government warehouse at the end of Raiders of the Lost Ark: There’s treasure in there somewhere, if only someone would look.
Other elite cancer research centers and genome-sequencing centers have similar in-house projects. Much like the NCI project, the unusual responder program at the University of Texas, MD Anderson Cancer Center, is beginning by combing through the archives to hunt for outliers of the past. A patient at the clinic who has an unusual response—good or bad—will also be referred for genome sequencing and other kinds of genetic analysis.
Even if each outlier case only applies to 3 or 7 percent of one type of cancer, as more cases are solved, the benefits quickly add up. “We’re talking about small subsets of patients that together make a radical change,” says Funda Meric-Bernstam, chair of the Department of Investigational Cancer Therapeutics at MD Anderson, who leads the unusual responders program. In some cases, existing cancer drugs can simply be repurposed, such as discovering that an immunosuppressant drug works for certain bladder cancers. Or it might mean finding new life for an experimental drug that had been abandoned. If Conley and Doroshow can pinpoint who might be helped by an abandoned drug, a pharmaceutical company might have to do just one or two further studies to get that drug approved for routine use.
The future might look something like what’s been going on for several years at the Genome Institute of Washington University, where genome sequencing is being used to help people with relapsed cancers and who have run out of options. The project puts insights from studies like Solit’s into practice, analyzing a patient’s tumor to determine whether currently available drugs might target the troublemaker mutations. Combining whole genome sequencing, exome sequencing, and RNA expression analysis—what Washington University professor of genetics and Genome Institute co-director Elaine Mardis calls the “Maserati approach”—the team compares a comprehensive genetic profile against a database of drugs that target specific gene variants, looking for a match.
If there is a match, the results can be impressive, as was the case with a young Washington University doctor with leukemia, Lukas Wartman, who had suffered two relapses. In his case, analysis revealed that a gene called FLT3 was expressing more RNA than normal. A drug that inhibits this gene, usually used in kidney cancer, sent his cancer into remission. Washington University now has a special genetic test for patients with his type of leukemia.
Just recently, Solit’s group solved another exceptional responder mystery—a case of ureteral cancer eliminated with a combination of old and new drugs. The old drug is a standard chemotherapy treatment that prevents DNA from unwinding, which it must do in order to duplicate itself during cell division. The new one sensitizes cells to the effects of radiation. This patient turned out to have a mutation in RAD50, involved in repairing broken DNA strands (badly repaired DNA can lead to uncontrolled cancerous growth). Here, too, the outlier finding may lead to a new treatment, since about 4 percent of the other tumors Solit has looked at have mutations that affect part of the RAD50 complex. “To look at these individuals’ cancers can tell us a lot more than just a random case of cancer,” says Solit. “There’s a phenotype—a response—that gives you information about the genes.”
Solit is now making a quick, reliable test for the TSC1 mutation to single out people with bladder cancer who might be helped by everolimus, and is planning a new study to test the drug in them. And the original outlier, the woman with bladder cancer? Three years later, she’s still on everolimus and still having a “complete response,” Solit says. She’s doing fine.
Kat McGowan is a contributing editor at Discover magazine and an independent journalist based in Berkeley, Calif., and New York City.