Three years later Daniel Kreitman still chokes up when he talks about what he saw, and how it changed him. Kreitman, an upholsterer by trade, had taken psilocybin, a hallucinogen derived from mushrooms, in a trial at Johns Hopkins University School of Medicine for nicotine addiction. He was 52, and he’d smoked between one and two packs a day for nearly 40 years. After his first psilocybin session, his urge to smoke was gone. During his third and final session, he had the vision that helped him quit for good.
He saw lakes, roads, and mountains, and a broad-shouldered man at the helm of a ship, lassoing birds. Was it his dead father? He wasn’t sure. But he remembers giggling and feeling good. Music was playing in his headphones. During Aaron Copland’s Appalachian Spring he had the sensation of physically touching the music, which was smooth and bright yellow in his mind’s eye. As the music progressed, he traveled, flowing outward toward an immense space that never ended. He may have wept for joy—he’s not sure—but the beauty of the vision overwhelmed him. “I was seeing forever,” he told me.

Kreitman was brought up Jewish, but doesn’t consider himself to be particularly religious. Yet he falls back on religious language to explain the experience. “I think I saw God at one point,” he said, his voice cracking with emotion. The day after the session, in his journal, he wrote: “The question is, if I saw God and infinity, what’s next? How does that change me and my life?”
When I spoke with him this August, Kreitman had an answer: He hadn’t had a cigarette for three years. He’d previously tried nicotine gum and patches, to no avail. He always returned to the habit, falling into the easy rhythms of smoking on the way to work and on the way home. It was taking a toll on his health, though. He was chronically short of breath and although they didn’t nag, his wife and children were concerned for his health. Since that session three years ago, however, cravings have barely registered. “It’s kind of crazy,” he told me. “I don’t feel like I’m fighting this addiction. It’s like it’s not even me.”
The trial was small, just 15 people, but it’s on the vanguard of resurgent research into the therapeutic potential of hallucinogens—a “psychedelic renaissance,” as one researcher described it. Work from the mid-20th century suggested that psychedelics held therapeutic promise. But those studies didn’t generally hew to modern scientific design.
Now, after decades of neglect, scientists are beginning to rigorously test hallucinogens as medicine. They’re trying to treat some of our most vexing afflictions, including addiction, depression, and the existential anxiety of having a terminal disease. The small studies so far conducted have yielded striking results. In one 10-person pilot study on alcoholics, participants more than halved their alcohol intake six months after taking psilocybin. In Kreitman’s study, 60 percent of smokers who took psilocybin hadn’t smoked two-and-a-half years later.
If hallucinogens prove effective in treating substance abuse, they would address a massive unmet need. They’d also possibly force a change in how we think about the dysfunction that underlies these conditions.
In the past, addiction was cast as a moral failing. Today it’s variously seen as a psychiatric condition, a learning disorder, or a disorder of the brain. Given that dependency on one’s drug of choice eventually emerges, a common treatment approach is to wean addicts off their drugs by, in the case of smoking, giving ever smaller quantities of nicotine in patches or gum.
Hallucinogen therapy dispenses with this gradualist approach, instead seeking a more sudden transformation. That’s in part because many studies, including the Johns Hopkins trial Kreitman participated in, suggest those who have mystical experiences while on psilocybin have the best outcome. This kind of sudden, divine-seeming insight, what William James termed a “conversion,” is central to many religious and meditative traditions. It can also occur in more prosaic contexts—a phenomenon one psychologist has dubbed “quantum change.” People can quickly and inexplicably, often after a profound epiphany, change.
He saw a broad-shouldered man at the helm of a ship, lassoing birds.
The question of how, precisely, hallucinogens trigger these transformations has sent neuroscientists down an intriguing rabbit hole. They have observed similarities between what happens in meditators’ brains and people on hallucinogens. Neural networks that serve as control centers—the neural correlates of the old Freudian ego—may loosen their grip, freeing other regions of the brain.
Researchers often use an unusual language to talk about this transformation, one that emphasizes meaning and subjective experience over molecular pathways and neurotransmitters. Hallucinogen therapy seems to recast addiction not only as a disorder of the brain, but as a disorder of meaning—of framing and how we see ourselves.
Ultimately, hallucinogen researchers are addressing a mystery that’s central to psychology and psychiatry, not to mention the self-help section of the bookstore: the question of how people change, of how they escape limiting and often self-destructive behavioral patterns. Their early research suggests that hallucinogen therapy offers a radically new perspective on the self, showing people that they’re not slaves to their compulsions or fears, and providing them with a sense of connection to something ineffable, something greater than themselves.
The psilocybin studies at Johns Hopkins University School of Medicine have been guided in part by Roland R. Griffiths, Ph.D., a professor in the departments of psychiatry and neuroscience at the university. About 15 years ago, Griffiths began meditating. He started with a Hindu mantra-based practice, and moved to Buddhism. As a scientist, he studied drugs of abuse—how they hooked people and why. But he’d always been curious about the nature of consciousness itself—why we’re aware at all—which is in many ways the fundamental enigma of human existence. He thought that meditation was one method, albeit a subjective one, for exploring this mystery.
As his meditation practice deepened, he began to have interesting and unusual experiences. They opened “a spiritual window,” he told me. “With meditation, one really begins to see how the mind works, how ideas come up.”
Seeking to better understand these experiences, Griffiths dove into the literature on comparative religion. There, he discovered claims that hallucinogens could induce experiences like those he had while meditating.
William James offered a compelling perspective on alternative consciousness in the early 20th century. “Looking back on my own experiences” with nitrous oxide (laughing gas), he wrote, “they all converge towards a kind of insight to which I cannot help ascribing some metaphysical significance. The keynote of it is invariably a reconciliation. It is as if the opposites of the world, whose contradictoriness and conflict make all our difficulties and troubles, were melted into unity.”
In the 1950s, scientists began exploring hallucinogens therapeutically. Humphry Osmond, a British-born psychiatrist working in Canada, conducted some particularly interesting work. Osmond, who coined the term “psychedelic”—“mind manifesting,” in his words—wanted to help alcoholics quit drinking. When longtime drinkers stop, they can suffer from a severe and occasionally deadly form of withdrawal called delirium tremens, which can include psychotic episodes. Delirium tremens also sometimes served as a turning point toward recovery in alcoholics’ lives. Only after they “hit bottom,” the thinking went, could they get better. Osmond and his colleagues reasoned that an LSD session, which also induces a psychosis-like state, might accelerate this naturally occurring process. He and his colleagues hatched a plan to treat alcoholics by inducing with megadoses of LSD the very psychosis they might experience down the road.
Hallucinogen therapy offers a radically new perspective on the self.
And it worked, sort of. Of his first two patients, one remained sober six months later. Over the years, Osmond and his colleagues treated perhaps 2,000 more drinkers with LSD, including many who hadn’t responded to other therapies, and achieved impressive results. Between 40 and 45 percent of his patients continued to abstain a year after treatment. It wasn’t that they were scared straight by their LSD episodes. Rather, over and over, these patients reported insightful and often mystical experiences—a feeling of being at one with the universe, and of seeing oneself and one’s internal conflicts clearly and objectively. Those experiences were central to their subsequent abstinence.
As it happens, Albert Hofmann, the Swiss scientist who first synthesized LSD, and who himself had an intense mystical experience while on the drug, had always hoped that his creation would be studied scientifically, its therapeutic potential rigorously tested. He once described LSD as “medicine for the soul”—as “a tool to turn us into what we are supposed to be.”
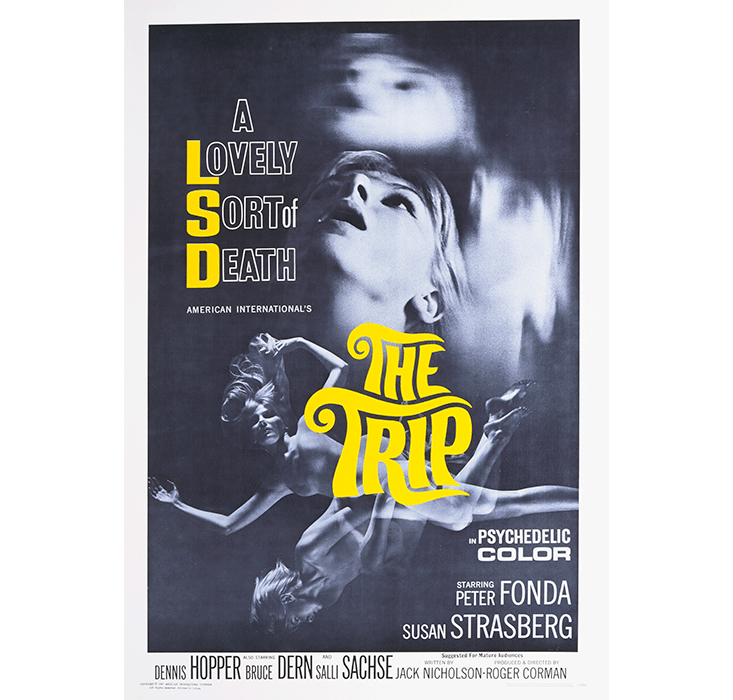
But by the late 1960s, research on hallucinogens mostly ground to a halt. The burgeoning counterculture got a hold of psychedelics—“altered consciousness” was a central aspiration of the movement—and a kind of anti-hallucinogen hysteria took hold among the establishment. Hallucinogens were linked to anti-war demonstrations and student riots. Newspaper articles began appearing claiming that LSD caused psychotic episodes, fetal abnormalities, and crime. The emerging evidence of therapeutic potential was dismissed as flawed, and the drugs were made illegal.
In the nearly 40 years since, establishment attitudes toward hallucinogens began to shift. Scientific curiosity began to displace hysteria. And in the early aughts, Griffiths decided to test the idea that hallucinogens could reliably provoke mystical experiences. He recruited 36 volunteers for a double blind study. No one knew exactly what drug conditions would be administered, and the stimulant Ritalin was given as a placebo.
He published his first results in 2006. Many participants reported having mystical-type experiences that, two months later, they rated as among the most meaningful of their lives. Nearly two-thirds of the participants said the experiences had increased their well-being—something that Griffiths and his colleagues confirmed with family and friends. Maybe most surprising, the subjects reported lasting change after the psilocybin sessions.
Psychologists often rate personalities in broad domain categories like neuroticism, extroversion, and agreeableness. After the age of 30, it’s thought that one’s personality is more or less set. But in Griffiths’ study, one domain in particular improved among the psilocybin-takers more than a year after the sessions: openness. They reported more imagination, creativity, and aesthetic appreciation.
It’s what many religious practices figured out long ago.
Others call these studies groundbreaking. They’re the first studies on hallucinogens in the U.S. in decades, and among the only rigorous studies ever. They suggest that mystical experiences are reliably inducible. And for Griffiths, they indicate that the human brain is wired to have these kinds of experiences. You don’t have to be a saint or a master meditator; you don’t have to be born lucky, or suffer from an unusual mental glitch. Perhaps because we’re extremely social animals, the ability to feel a deep sense of oneness with existence, which seems so therapeutic, is latent in us. “The results suggest that almost everyone is capable,” he told me.
It also makes hallucinogens easier to study, and easier to administer as therapy. That’s not to say that everyone who takes hallucinogens will feel at one with the universe, or see their version of God. The lead-up to the sessions is, Griffiths believes, important to the outcome. He and his colleagues put a lot of thought into creating a setting that they think increases the odds of a positive session. Kreitman began preparing for about two months before his psilocybin sessions. He learned to meditate, talked with a psychologist regularly, and developed a mantra—“For myself and my family, I quit for life”—meant to crystallize his intent to stop smoking.
On the day of his first session, after crushing and throwing away his last pack of cigarettes, he lay back on a comfortable couch in a warmly lit room decorated with Buddha statues, pulled a blinder over his eyes, and listened to pleasant, occasionally Indian-sounding music on earphones. Doctors monitored him, periodically asking how he was doing and taking his blood pressure. “It was comforting to know they were watching me,” Kreitman said.
Post-psilocybin, Kreitman describes himself as the same, but also “deeper.” And this newfound depth occasionally manifests in the strangest way: a tendency to spontaneously weep, not with sadness, but with joy. “It’s great,” he told me. “But my kids think I’m losing it.”
When you imbibe psilocybin, your body metabolizes it into psilocin, the active compound in the hallucinogen. Psilocin and LSD both stimulate serotonin receptors on neurons, exciting those cells and prompting a cascade of secondary activity. Serotonin is often described as a mood regulator, important to one’s happiness and sense of well-being. Many antidepressant drugs also boost serotonin levels in the brain. Yet this biochemical understanding doesn’t quite explain the subjective experience of “the trip,” or the effects that continue long after hallucinogens have left the body.
It’s from neuroscience that the most alluring and potentially informative portrait of what happens to the brain on psychedelics has begun to emerge. Scientists at the University of Zurich have found that activity in the amygdala, the fear center of the brain, declines on psilocybin, making people less reactive to negative stimuli, which might explain how it could help with depression.

A series of studies by scientists at Imperial College London indicate that while people are on hallucinogens, connectivity within neural networks responsible for weaving information into a coherent whole declines; but connectivity between networks usually specialized in different tasks increases. What that implies is both a kind of disorder—the kaleidoscopic colors and sensation of dreaming while awake—and a kind of freedom, which the researchers call “ego dissolution.”
“Under the influence of psilocybin, there’s more crosstalk across networks. Brain activity is less tightly organized,” Michael Bogenschutz, a scientist at New York University who’s conducting a study on alcoholics, told me. “It’s consistent with people’s subjective reports of synesthesia”—smelling colors, seeing flavors, and a general sensory confusion—“and perceiving connections between things that don’t ordinarily appear to be related.”
One of the networks where activity declines is the “default mode network.” It’s important for internally directed activity like rumination and daydreaming, and includes neural hub areas like the parahippocampus (involved in spatial recognition), the posterior cingulate cortex and precuneus (imagining oneself in the future or the past), and the medial prefrontal cortex (autobiographical memories).
The default mode network usually operates in opposition to another network associated with externally oriented tasks, like playing soccer or hunting deer, called the “task positive network.” These two separate neuronal webs tend to operate like a seesaw: When one is activated, the other is muted, and vice versa.
But when volunteers took psilocybin, the Imperial College scientists found, both networks activated simultaneously—a pattern also observed in experienced meditators. Brain scans of people on hallucinogens, as with meditators, have revealed that the concurrent activation of these networks predicts a loss of one’s sense of separateness—the ego—and the emergence of a feeling of profound interconnectedness.
By loosening the inner tyrant, hallucinogens impart a lightness of being.
LSD also causes the default mode network to fragment slightly, while boosting activity between other usually segregated areas. The parahippocampus and another region called the dorsomedial prefrontal cortex, important in that sense of “me-ness,” begin talking more, even as the posterior cingulate cortex and the parahippocampus—two hubs of the default mode network—talk less.
The Imperial College scientists interpret these findings as evidence that regions of the brain charged with executive control and top-down maintenance of order—the “rich club,” they call it—relax their grip. The usual separation of brain regions and their functions collapses, and a kind of neural cosmopolitanism emerges. It’s tempting to imagine that, with the proverbial parents out of town, the brain throws a wild, teenage party—that what happens during an LSD trip is a bottom-up explosion of usually repressed exuberance.
This explanation gets at one of the more fascinating models of brain function. Making sense of the world may require the brain to restrain itself—to limit how and what it perceives. In a Darwinian sense, it’s obvious why that imposition of order might be necessary. If you constantly experienced the world as an acid trip, unable to distinguish your imagined dragons from that very real tiger waiting to pounce, you probably wouldn’t last long. But it’s also possible that the imposition of order can, when it becomes too iron-fisted, imprison us psychologically. So by taking those punctilious, literal-minded “hubs” offline, hallucinogens may free up other brain regions and their associated talents, enabling “a state of unconstrained cognition,” as the scientists put it, and ultimately liberating us from ourselves.
In the neuroscience literature, case reports on stroke, trauma, and even dementia victims suggest that damaging one part of the brain can indeed lead to dramatic enhancements in creativity and well-being, likely by freeing other regions of the brain and their creative energies. Hallucinogens may do something similar, not by destroying those parts of the brain, but by momentarily weakening their hold over other areas.
Still, that doesn’t explain how hallucinogens, which are taken for just a few sessions, can induce lasting changes—like Kreitman’s three-year abstinence from cigarettes. Most psychotropic drugs, such as SSRIs, must be taken chronically to work. The medication needs to be in your system to have its effect. By contrast, the effect of hallucinogens seems to continue long after they’ve left your body.
Bogenschutz hypothesizes that hallucinogens open a window of enhanced neural plasticity, the brain’s inherent ability to change. Networks of neurons, connected by branch-like filaments, underlie everything you think and feel. Rather like heat makes metal malleable, hallucinogens might enable and accelerate the formation of new connections between neurons, allowing you to alter the prison of your bad habits, fears, and compulsions. And if the mystical experience is important in this plasticity—Bogenschutz says “more work will be necessary to determine if that is indeed the case”—the implication is that the drug alone isn’t what’s important, but rather the subjective experience while on the drug.

As evidence that such a thing is even possible—that intense experience can rewire connections in the brain—Bogenschutz points to post-traumatic stress disorder. There are measurable differences in brain and immune function in people suffering from the condition, changes prompted by trauma that’s not necessarily physical, but experiential.
“In PTSD, it’s the intense emotional response generated by what you perceive is happening” that induces these changes, Bogenschutz says. “It’s mediated not just by the experience itself, but by the meaning attached to that.” Why, then, couldn’t an extraordinary experience of great significance push you in a more positive direction—toward, say, an epiphany that helps you stop smoking?
For his part, Griffiths sees hallucinogens as a crash course in the nature of mind, “which may be relevant to what meditation and religious traditions have explored,” he said. Many forms of meditation exercise the ability to observe the mind without becoming trapped in what’s happening. With time, strengthening this skill may result in a lightness to one’s day-to-day activity, a non-attachment that practitioners often describe as liberating. Perhaps by loosening the grip of the inner tyrant, hallucinogens impart a similar “lightness of being,” as Griffiths calls it. That kind of “efficacy”—the ability to avoid becoming entangled in your own fickle desires—is probably essential to abstinence, he says. Post-psilocybin, patients “are not so worried about their addiction of cravings,” Griffiths told me. “They know that it will pass.”
Nearly a century ago, an alcoholic named Bill Wilson was lying in bed, in a hospital, struggling mightily with his lifelong depression. At wits’ end, he reportedly cried out, “I’ll do anything! Anything at all! If there be a God, let Him show Himself!” at which moment, he saw a bright light—he’d later call it a “hot flash”—was overcome by a feeling of ecstasy, and a great sense of peace.
He never drank again.
Wilson went on to found Alcoholics Anonymous, the well known recovery and abstinence program.1 At some point, Wilson became interested in LSD as a way to help alcoholics quit drinking. He tried it himself, and, like Osmond, thought it might induce in others the experience that had helped him. What Wilson’s story makes clear, however, is that people can naturally and spontaneously have epiphanic experiences that help them quit drinking.
Will Miller, an emeritus psychologist at the University of New Mexico in Albuquerque, has dubbed these sudden psychic shifts “quantum changes.” He began studying them after his own troubled daughter had an epiphany, and transformed into a caring, responsible woman seemingly overnight. These stories present certain commonalities, he says: an intense sense of interconnectedness; the sudden awareness that one’s sense of isolation is an illusion; the realization that others’ shortcomings should be met with compassion, not judgment and punishment. People find sudden release from addictions and dependencies. They repair broken relationships. “I think of it as an evolution in consciousness,” Miller told me. He added, “dramatic change is possible. We’re not stuck in yesterday.”
But these sudden transformations were completely unpredictable. Miller couldn’t pinpoint any characteristics that foretold who might experience them, or when. The hallucinogen research needs replication precisely for this reason. If you could induce “quantum change” reliably, you can study it. And imagine the potential benefit not just for addicts, but for everyone.
Assuming that addiction research continues to show promise, Griffiths foresees hallucinogens used in clinical settings that, like his own studies, offer extensive pre- and post-treatment support. Griffiths doubts that hallucinogen therapy will spread anytime soon, however, not because it’s a bad idea, but because we have a strong cultural bias against performance-enhancing drugs. “Right now, the idea of giving drugs to improve the betterment of all people would strike at least some people as repugnant,” he told me.
But in 20 years, who knows? By then, we may have more precise approaches to induce the same shifts, such as transcranial magnetic stimulation or even precision brain surgery. For Griffiths, hallucinogens’ primary contribution may be as a teaching tool, a way to learn how human transformation works so we can encourage it by other methods with fewer potential side effects. The lesson for now, he said, is simply that profound metamorphosis is possible. “We do appear to be biologically predisposed to have experiences that can be the pivot point for enduring radical behavioral change in personality, attitudes, and behavior.”
Moises Velasquez-Manoff is a journalist and author of An Epidemic of Absence: A New Way of Understanding Allergies and Autoimmune Diseases.



























