Safe, effective, and available vaccines are the best long-term solution to the coronavirus pandemic.1 So it’s welcome news that two vaccines are poised for distribution and others will soon be on their way. Preliminary clinical trial data from these two vaccines, made by Pfizer and Moderna, indicate the vaccines are effective at stimulating a strong and long-lasting response against the virus responsible for COVID-19. A recent FDA briefing2 confirmed the efficacy and safety profile of Pfizer’s vaccine, reiterating the shot was 95 percent effective at preventing COVID-19 after two doses with no serious safety concerns.
This is all good news, but it’s still unlikely that a vaccine will be widely distributed until mid 2021. Supply constraints could cause additional delays.3 In the meantime, health professionals must continue to develop, trial, and improve the therapeutic management of COVID-19, and people must continue to attenuate transmission through social distancing and adherence to recommended public health practices such as wearing a mask and avoiding crowded indoor activities.
Fear of a disease does not always translate into high vaccination rates.
Looming over our best efforts, however, is a factor that could derail the campaign to end the pandemic: distrust of vaccines. In a survey of 1,000 individuals in New York City in April 2020, at the height of the epidemic’s first wave, only 59 percent of respondents said they would get a vaccine, and only 53 percent would have their children vaccinated.4 The large public and private investments in developing vaccines need to be matched by investments in laying the groundwork for vaccine acceptance.
Much is at stake. If the vaccination roll out is to succeed, it behooves us to be sensitive to general perceptions about vaccination. COVID-19 vaccination has to be viewed within the broader context of attitudes toward routine immunization. An effective and safe vaccine that stops the pandemic and restores our ability to resume social, educational, and economic activity could improve public attitudes toward science and enhance vaccine acceptance more generally. Issues around public acceptance of COVID-19 vaccination could influence immunization campaigns for years to come.
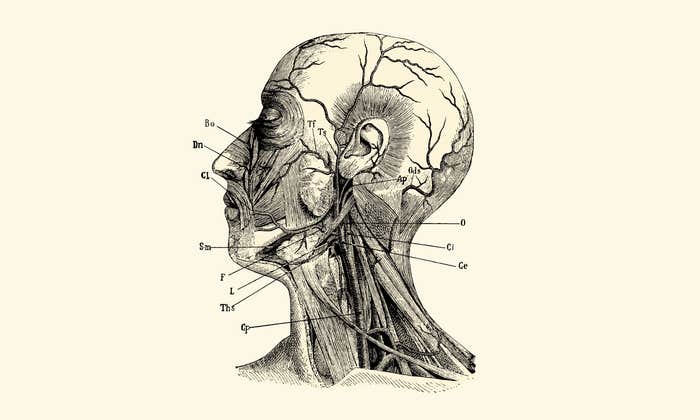
Vaccine hesitancy in the United States now ranges from narrow concerns about specific vaccines to broad coalitions of “anti-vaxxers” who reject all vaccines. The roots of these sentiments, most without scientific basis, run deep. The continual expansion of vaccines for children (from seven vaccines 40 years ago to 15 today) is mistakenly thought to burden young immune systems. Other factors include suspicion about the financial motives of the vaccine industry, mistrust of scientific evidence and government institutions,5,6 the effect of vaccine vehicles on neurological disorders, and the distrust in vaccines deliberately sown by Russian-linked social media accounts.7 The result: Even though annual flu shots are available at most neighborhood pharmacies, fewer than half of Americans now receive a flu shot each year.8
Reluctance to get vaccinated for COVID-19 is widespread. Only two-thirds of crowdsourced participants (68.2 percent) in a survey of Canadians reported being very likely to voluntarily get vaccinated.9 In Israel, people who had received influenza vaccinations in regular years were more likely to report that they would accept a COVID-19 vaccine, but others were hesitant.10 A nationally representative study in Ireland and the United Kingdom reported vaccine hesitancy for 26 percent and 25 percent of respondents, and resistance for 9 percent and 6 percent, respectively.11 A survey of 450 Americans found that 67 percent would accept a COVID-19 vaccine if one were recommended by the government. Males (72 percent), adults over 55 (78 percent), Asians (81 percent), and college and/or graduate degree holders (75 percent) were more likely to accept a vaccine.12 Other surveys have indicated that 35 percent of Americans would not accept a COVID-19 vaccine even if one were available today.13
Mandatory vaccination should be avoided. Vaccination status should be tied to travel or access to public places.
Vaccine hesitancy may not be uniform for all age groups. Parents are more reluctant to vaccinate their children than themselves,14 but children have been found to be key spreaders of infection and should arguably be among the priority groups to be vaccinated, especially if the antibody response is weak in the elderly population.
Attitudes toward a COVID-19 vaccine are still evolving. People’s preferences are a function of the perceived safety and efficacy of a vaccine, and the health burden and outcomes related to the disease—both of which could change. The virus may mutate and become less (or more) virulent. An effective therapeutic may depress the perceived need to be vaccinated, since individuals in good health are often willing to risk getting ill and receive treatment rather than get a vaccine. Risk-benefit calculations may be shaped by new information on the long-term respiratory and neurological effects of the virus. People worldwide may develop pandemic fatigue and desire only a return to normalcy.
The perceived risk posed by the infectious agent is a major motivator for vaccination,15 and this works in favor of acceptance of a COVID-19 vaccine. Perceptions of personal vulnerability16 and anticipated regret17 are also correlated with the choice to be vaccinated, and both are likely to be high for this disease. The more effective the COVID-19 vaccine, the more likely people will choose to be vaccinated. Paradoxically, however, this could reduce vaccine uptake over time if the incidence of COVID-19 declines.18 Fear of a disease does not always translate into high vaccination rates, as a study of tetanus in the 1960s showed.19
Widespread vaccination against COVID-19 requires that scientists and healthcare workers go beyond just providing information: The issue is not simply a matter of educating people about the importance of vaccination. A more sophisticated approach is needed to address convenience, affordability, and trust in public institutions.
The first hurdle is engendering confidence in the vaccine development process. The speed at which the first vaccines have been developed could itself prove a barrier to vaccine acceptance. The language of “Warp Speed,” intended to communicate urgency, unintentionally signals a prioritization of urgency over safety. In this context, the commitment of pharma CEOs to “only submit for approval or emergency use authorization after demonstrating safety and efficacy through a phase 3 clinical study that is designed and conducted to meet requirements of expert regulatory authorities such as FDA” inspires confidence.20 The advantages of getting a vaccine to market quickly could be squandered if too many people believe it has been rushed to market without adequate safety and efficacy testing. Time is wasted if they need to be convinced otherwise. Communicating the vaccine’s safety and efficacy is critical. Without this, even healthcare workers may be reluctant to be vaccinated.10
Second, trust in public authorities is likely to be a significant factor.10 People with diminished trust in the country’s leaders are far less likely to accept a COVID-19 vaccine. Public officials, community leaders, celebrities, and their families should themselves get vaccinated and be transparent in a nonlegalistic, commonsensical manner about the risks and benefits. Trusted voices must be used to improve public understanding. The enthusiastic declaration by three former U.S. presidents that they want to be among those receiving the vaccine will hopefully inspire other influencers to step forward.
Third, it is important to find local solutions to vaccine hesitancy. Demographic and geographic disparities in vaccine acceptance could lead to creating clusters of unvaccinated individuals who could then sustain repeated outbreaks of COVID-19. Achieving a high national average vaccination coverage rate would then not be sufficient. A targeted approach to messaging and improving coverage could expedite our exit from the pandemic.
Surveys have indicated 35 percent of Americans would not accept a COVID-19 vaccine.
Fourth, mandatory vaccination policies should be avoided because they could backfire. More acceptable would be tying vaccination status to travel or access to public places. Such policies preserve individual agency to reject the vaccine while also protecting public health, much like regulations that prohibit smoking in public places: Individuals can do as they like in private.
Finally, social media should be used to help shape preferences around COVID-19 vaccination and counter those who oppose vaccines under any circumstances. Researchers found that 54 percent of anti-vaccination ads on Facebook came from just two organizations: the World Mercury Project and Stop Mandatory Vaccinations.21 Facebook’s recent pledge to remove discredited claims about COVID-19 vaccinations22 could be a significant step toward countering misinformation from these groups, despite the inherent difficulties around detecting, discerning, and removing misinformation at scale.23
Another study24 found that anti-vaccine groups were small and had few followers but were more likely to be linked into social media of decision-making bodies, such as parent associations at schools. Emotive and fear-based online messages are seeding doubt about vaccines and gaining disproportionate strength over neutral, scientific postings.
There is little time to lose in the campaign to end the pandemic with a vaccine. At least 70 percent of the population must be covered to reach herd immunity, with higher or lower levels in some communities. This is achievable. Mississippi, with strict laws against nonmedical vaccine exemptions for school attendance, has vaccination rates for measles and diphtheria-tetanus-pertussis exceeding 99 percent, and California, Maine, and West Virginia have followed the Mississippi example. Successful vaccination programs are possible in all states, regardless of the political leanings of their residents.
Fresh thinking and behavioral research are needed to build trust and complement authoritative and data-oriented communications. A lot has been written on the importance of known, trusted messengers of information including doctors and nurses, community thought leaders like ministers, or heads of important community groups. However, our existing knowledge base is in the context of childhood vaccines. Trusted voices and strategies to support a potential COVID-19 vaccine need to be identified. Discussions with family and friends can help address people’s concerns, yet this is not part of the current strategy to encourage vaccination.25 There is evidence that traditionally trusted sources like the U.S. Centers for Disease Control and Prevention are seen as less reliable in the context of a COVID-19 vaccine than are doctors and nurses.26 Given the importance of community opinions and social norms, vaccine messaging and engagement should address specific communities known for low vaccination compliance.27 We have a window of opportunity to course correct to ensure that we have a vaccine that is not just safe, effective and available but is also trusted. That work should begin immediately.
Ramanan Laxminarayan is an economist and an epidemiologist. He is founder and director of the Center for Disease Dynamics, Economics & Policy in Washington, D.C., senior research scholar at Princeton University, and an affiliate professor at the University of Washington.
Susan Fitzpatrick is president of the James S. McDonnell Foundation, a member of the Santa Fe Institute’s Science Board and a voluntary faculty at Washington University and Arizona State University. Her work is dedicated to encouraging the application of scholarly knowledge to important societal problems.
Simon A. Levin is the James S. McDonnell Distinguished University Professor in Ecology and Evolutionary Biology at Princeton University, the director of the Center for BioComplexity, and a member of the Santa Fe Institute’s Science Board. His research interests are in understanding how macroscopic patterns and processes are maintained at the level of ecosystems and the biosphere.
Acknowledgement: We are grateful to the James S. McDonnell Foundation for its support through Princeton University to support a collaborative addressing vaccine hesitancy and other public health issues. We also thank Aditi Sriram at CDDEP for valuable research assistance. Any errors that remain are the sole responsibility of the authors.
References
1. Leung, K., Wu, J.T., Liu, D., & Leung, G.M. First-wave COVID-19 transmissibility and severity in China outside Hubei after control measures, and second-wave scenario planning: a modeling impact assessment. Lancet 395, 1382-1393 (2020).
2. PFIZER-BIONTECH COVID-19 VACCINE (BNT162, PF-07302048) VACCINES AND RELATED BIOLOGICAL PRODUCTS ADVISORY COMMITTEE BRIEFING DOCUMENT- FDA.gov. Accessed Dec. 8, 2020. https://www.fda.gov/media/144246/download
3. Sheikh, K. Find a vaccine. Next: Produce 300 million vials of it. The New York Times (2020).
4. COVID-19 Tracking Survey, School of Public Health. Accessed August 13, 2020. https://sph.cuny.edu/research/covid-19-tracking-survey/
5. Salmon, D.A., Dudley, M.Z., Glanz, J.M., & Omer, S.B. Vaccine hesitancy: Causes, consequences, and a call to action. Vaccine 33, D66-D71 (2015).
6. Larson, H.J., Cooper, L.Z., Eskola, J., Katz, S.L., & Ratzan, S. Addressing the vaccine confidence gap. Lancet 378, 526-535 (2011).
7. Walter, D., Ophir, Y., & Jamieson, K.H. Russian twitter accounts and the partisan polarization of vaccine discourse. American Journal of Public Health 110, 715-724 (2020).
8. Flu vaccination coverage, United States, 2018–19 influenza season | fluvaxview | seasonal influenza (Flu) | CDC. Accessed August 25, 2020. https://www.cdc.gov/flu/fluvaxview/coverage-1819estimates.htm#summary
9. Concerns about COVID-19 — A view from Canada — Coronavirus (Covid-19) researches. Accessed August 10, 2020. https://researchchoices.org/covid19/findings/report/41/concerns-about-covid-19-april-13-2020
10. Dror, A., et al. Vaccine Hesitancy: The next challenge in the fight against COVID-19. European Journal of Epidemiology 35 (2020).
11. Murphy, J., et al. Preparing for a COVID-19 vaccine: Identifying and psychologically profiling those who are vaccine hesitant or resistant in two general population samples. PsyArXiv (2020).
12. Malik, A.A., McFadden, S.M., Elharake, J., & Omer, S.B. Determinants of COVID-19 vaccine acceptance in the US. medRxiv (2020).
13. Mullen O’Keefe, S. One in three Americans would not get COVID-19 vaccine. News.gallup.com (2020).
14. Lima, G., Hwang, H., Cha, C., & Cha, M. Public willingness to get vaccinated against COVID-19: How AI-developed vaccines can affect acceptance. arXiv (2020).
15. Brewer, N.T., et al. Meta-analysis of the relationship between risk perception and health behavior: The example of vaccination. Health Psychology 26, 136-145 (2007).
16. Brewer, N.T., DeFrank, J.T., & Gilkey, M.B. Anticipated regret and health behavior: A meta-analysis. Health Psychology 35, 1264-1275 (2016).
17. Brewer, N.T., Chapman, G.B., Rothman, A.J., Leask, J., & Kempe, A. Increasing Vaccination: Putting psychological science into action. Psychological Science in the Public Interest 18, 149-207 (2017).
18. Leventhal, H., Singer, R., & Jones, S. Effects of fear and specificity of recommendation upon attitudes and behavior. Journal of Personality and Social Psychology 2, 20-29 (1965).
19. Frank, K. & Arim, R. Canadians’ willingness to get a COVID-19 vaccine when one becomes available: What role does trust play? www150.statcan.gc.ca (2020).
20. Taylor, N.P. COVID-19 vaccine CEOs vow to wait for phase 3 data before filing for approval. fiercebiotech.com (2020).
21. Jamison, A.M., et al. Vaccine-related advertising in the Facebook Ad archive. Vaccine 38, 512-520 (2020).
22. Isaac, M. Facebook says it will remove coronavirus misinformation. The New York Times (2020).
23. Bliss, N., et al. An Agenda for Disinformation Research. Computing Community Consortium (CCC) Quadrennial Paper [whitepaper]. (2020) https://cra.org/ccc/wp-content/uploads/sites/2/2020/11/An-agenda-for-disinformation-research.pdf
24. Johnson, N.F., et al. The online competition between pro- and anti-vaccination views. Nature 582, 230-233 (2020).
25. Chan, M.S., Jamieson, K.H., & Albarracin, D. Prospective associations of regional social media messages with attitudes and actual vaccination: A big data and survey study of the influenza vaccine in the United States. Vaccine 38, 6236-6247 (2020).
26. Reed, T. Americans see hospitals as more trustworthy than FDA or CDC on COVID-19 vaccine information, poll finds. fiercehealthcare.com (2020).
27. Quinn, S.C., et al. The influence of social norms on flu vaccination among African American and White adults. Health Education Research 32, 473-486 (2017).
Lead image: Leremy / Shutterstock