Jane McKeating never expected time to matter much in the liver.
About a decade ago, McKeating was examining medications to use during liver transplantation in patients with chronic hepatitis C infections. Hepatitis C can linger in the body for decades and cause severe liver damage—and in those days, the lack of drugs to combat the viral infection meant that when a patient received a replacement liver, the virus could immediately infect the new organ. McKeating, then a virologist at the University of Birmingham in the United Kingdom, and her colleagues wanted to see whether an antiviral drug could stop the virus’ spread and save the new livers.
Hidden inside most of our cells are so-called clock genes.
When the team initially assessed their data, they were stumped. It looked like the drug prevented infection in some patients, but not others—and it wasn’t clear what, exactly, was behind this difference.
“We just couldn’t understand what was discriminating between the patients,” says McKeatin, now at the University of Oxford. After much head scratching, they noticed a perplexing pattern: Patients who received their liver transplants in the morning were more likely to be reinfected with the hepatitis C virus than those who had their operations in the afternoon.1 “It turned out it was the time of day when they received the liver transplant,” she says.
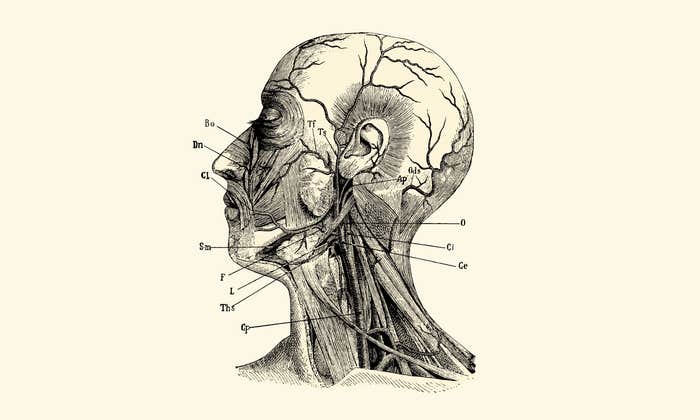
Each day, the Earth transitions through periods of daylight and darkness in time with the planet’s rotation around the sun. Many of our bodily functions follow the 24-hour cycles known as circadian rhythms. In addition to the daily cycles of sleep and wakefulness, many other processes within our body—such as the regulation of our internal temperatures, the release of hormones, when we digest our food—are also under circadian control. Hidden inside most of our cells are so-called clock genes that regulate the timing of cellular activities. Researchers have found that nearly half of our protein-producing genes work in a time-dependent manner.2 These pacemakers throughout the body are coordinated by the suprachiasmatic nucleus, a master clock in the brain.
Circadian biology was not part of McKeating’s research repertoire when she conducted her liver transplantation study. But after seeing these strange results, she knew she needed to investigate further. So she, along with Alan Zhuang, a postdoctoral researcher in her lab, set up an entirely new program to study the chronobiology—the science of circadian rhythms—of viruses.
In the years since, her team has investigated a range of viruses, from hepatitis to SARS-CoV-2, uncovering ways in which biological rhythms influence these pathogens, and vice versa.
Their work is part of a burgeoning area of research revealing that circadian cycles orchestrate many crucial functions of the immune system. And that these daily cycles can play a role in determining the outcome of viral infections, autoimmune disease, and other conditions—such as cancer—that involve the body’s defenses.
“If you look at pretty much any immune cell and its core functions, and you ask: ‘Does it change or can it be affected with circadian rhythms?’ The answer is ‘yes,’” says Jacqueline Kimmey, an investigator at the University of California, Santa Cruz.
The physician-scientist Franz Halberg coined the term “circadian” in 1959, following years documenting rhythmicity he saw in biological processes that paralleled the time cycles in nature. Among his many observations was the discovery that the outcome of an infection depended on when an exposure to a pathogen occurred.
In 1960, Halberg and his colleagues at the University of Minnesota conducted a simple experiment: They injected pieces of Escherichia coli bacteria known as lipopolysaccharides—toxins located on the outer layer of microbes—into the stomach of mice at different times of day.
They found that how the animals fared was highly dependent on when they had received the toxins: Mice injected during the evening, when they’re typically awake and active, were much more likely to survive than those injected during daylight hours, when the rodents were at rest. Other research groups subsequently found similar time-of-day dependent reactions in mice infected with another bacterium, Streptococcus pneumoniae.
Circadian rhythms within the immune system may be relevant beyond infections and autoimmune diseases.
More than a decade later, Halberg was part of a group of researchers who pinpointed another aspect of immunity influenced by daily rhythms: responses to vaccinations. In a 1976 study, the team used red blood cells from sheep as antigens—molecules that will prompt an immune response—in mice. Several days later, they observed that strength of the immune response the animals generated was dependent on the time of day when they received their inoculations.
These early studies indicated that innate immunity—the body’s first-line defense against pathogens and other harms—and adaptive immunity—the slower acting but more specific response system—had unexpected cycle-dependent responses. But the molecular underpinnings of these links remained mysterious.
Beginning in the early 2010s, scientists began uncovering some of this unseen orchestration. In one study, Louise Ince, who was then a postdoctoral researcher in the lab of Christoph Scheiermann at the University of Geneva in Switzerland, examined how the time of day influenced how dendritic cells—cells involved in triggering adaptive immune responses—migrate to lymph nodes, the small structures that help filter out and fight pathogens. The cells were more mobile when injected during the day, when the mice were at rest, than at night, when they were active. “You can really see that the amount of cell migration is significantly different depending on the time that you give the injection,” Ince says.
After observing this effect, the team decided to investigate whether responses to vaccinations would show similar time-dependent responses. When they inoculated mice with the hepatitis A vaccine, they found that giving the animals the shot during their resting phase, rather than their active phase, led to stronger responses in several immune cells, such as T cells—key players in adaptive immunity. Those findings were published earlier this year.3 Why immune cells appear more active during rest remains to be determined, but some researchers speculate that enhancing immunity before rising may prepare organisms to fight off pathogens they may encounter while awake.
McKeating’s team has been looking at how the viruses themselves are influenced by these biological rhythms. Her lab has been studying various viruses, primarily within cells in a dish, to get a closer look at this process in a variety of different pathogens. In their studies of hepatitis B—which, like hepatitis C, can cause chronic infection with the liver—the researchers have found that fragments of the virus’s DNA can interact with clock proteins within our cells and that the clock system can regulate viral replication.4 Preliminary work conducted by one of McKeating’s Ph.D. students, Helene Borrmann, on another long-lingering pathogen—human immunodeficiency virus, or HIV—suggests that the replication of this virus is also modulated by circadian rhythms.
During the pandemic, her group also took a look at SARS-CoV-2, the virus behind COVID-19, and found that a key component of the circadian clock can alter the virus’s ability to enter and replicate within lung cells.5 “There is this fascinating interplay between the virus and the clock system,” her colleague Zhuang says. But this interaction is complex, he adds, and how exactly it occurs depends on the virus. In viruses like hepatitis and HIV, it appears that perturbing the cellular clock hinders viral replication, while in others like influenza, disturbing the clock appears to have the opposite effect. “Every virus is different,” he adds.
While much of the experimental work has been done in animals or cells in a lab dish, scientists have also been gathering evidence for time-of-day effects in humans.
Echoing Halberg’s work in mice nearly half a century ago, several recent studies have found that timing influences the effectiveness of human-targeted vaccines.6 One clinical trial of older adults in the U.K. who received seasonal influenza vaccines in the morning experienced a greater increase in antibodies, for example, than those who received the shot in the afternoon. Researchers have reported similar findings for vaccines against other pathogens, such as Mycobacterium tuberculosis (the bacterium that cause tuberculosis) and SARS-CoV-2.
Support for the notion that the time-of-day a vaccine is administered influences its ability to protect against infectious disease is growing, Zhuang says. But the majority of human studies to date have looked mainly at antibody responses—and researchers will need to look at whether timing affects other immune cells to determine how much of an effect on long-term immunity timing really has.
Timing influences the effectiveness of vaccines.
Other curious observations in people have also spurred further investigations. Clinicians have long known that symptoms of rheumatoid arthritis, an autoimmune disease, tend to flare up in the mornings. This pattern is so widely accepted that it is one of the factors used to diagnose the disease, says Julie Gibbs, a professor at the University of Manchester who studies the circadian control of inflammation.
Gibbs and her group have been focused on looking at how and why the symptoms of immune-linked disease like rheumatoid arthritis fluctuate at different times of day. In mice, they’ve found that a specific type of immune cell responsible for dampening inflammation known as regulatory T cells within joints are fewer in number at periods when symptoms peak. They’re now planning to gather samples from patients to see whether the same is true in humans—with the hopes of one day being able to harness whatever is driving the accumulation of regulatory T cells in order to help treat the disease. Perhaps coaxing these T cells to report to work in joints at specific times of day can prevent inflammation from taking hold.
Ultimately, circadian researchers hope to be able to capture what they’ve discovered to improve immune-based treatments—such as medications for autoimmune disease and immunotherapies for cancers—and preventions, such as vaccinations. Many also hope to one day develop drugs that Zhuang describes as “clocks in a bottle,” which could manipulate circadian rhythms in beneficial ways.
The universe of time inside the body is still largely mysterious, however. Scientists have not discovered how, exactly, immune cells’ circadian rhythms are determined—and how they talk with the central clock in the brain. They have a hunch that circadian rhythms within the immune system may also be relevant beyond infections and autoimmune diseases. For example, researchers have recently found a role for these cycles in cancer. In a mouse study from late 2022, Scheiermann and his team demonstrated immune cells’ ability to track down and destroy cancer cells depended, yes, on the time of day.7 The cells were much better defenders during daytime, the animals’ resting phase.
McKeating, who began her research career studying HIV, says that when she thinks back to the long line of failed vaccines in this field, she wonders whether timing may have been a key factor that was previously ignored. Moving forward, she says, both scientists and clinicians need to be more cognizant of time: tracking when experiments are done, and when drugs are given. “I think all of this is really relevant going forward,” she says. “This is an exciting area of biology that I think will grow.” And, she says, certainly more will reveal itself with time. ![]()
Diana Kwon is a Berlin-based science journalist who covers health and the life sciences. Her work has appeared in Scientific American, Nature, The Scientist, among other publications. You can find her at www.dianakwon.com and @DianaMKwon.
Lead image: Lightspring and Siberian Art / Shutterstock
References
1. Zhuang, X., Lai, A.G., McKeating, J.A., Rowe, I., & Balfe, P. Daytime variation in hepatitis C virus replication kinetics following liver transplant. Wellcome Open Research 3 (2018).
2. Ruben, M.D., et al. A database of tissue-specific rhythmically expressed human genes has potential applications in circadian medicine. Science Translational Medicine 10 (2018).
3. Ince, L.M., et al. Influence of circadian clocks on adaptive immunity and vaccination responses. Nature Communications 14, 476 (2023).
4. Zhuang, X., et al. Circadian control of hepatitis B virus replication. Nature Communications 12, 1658 (2021).
5. Zhuang, X., et al. The circadian clock component BMAL1 regulates SARS-CoV-2 entry and replication in lung epithelial cells. iScience 24, 103144 (2021).
6. Otasowie, C.O., Tanner, R., Ray, D.W., Austyn, J.M., & Coventry, B.J. Chronovaccination: Harnessing circadian rhythms to optimize immunization strategies. Frontiers in Immunology 13 (2022).
7. Wang, C., et al. Dendritic cells direct circadian anti-tumor immune responses. Nature 614, 136-143 (2023).