On May 27th, the Pentagon admitted that it had shipped live anthrax to facilities in multiple U.S. states, and to a U.S. airbase in South Korea—by accident. Anthrax is usually kept in highly secure biolabs with multiply redundant safeguards. But we’ve always known there is room for human error.
The history of the biolab revolves around events like those of 1921, when two French scientists presented the world with a powerful weapon against tuberculosis. “The Great White Plague,” as it was called, had been infecting and killing humans with relative impunity for over 5,000 years before Albert Calmette and Camille Guérin unveiled their vaccine, composed of weakened tubercle bacteria. The vaccine caused mortality rates to fall, but its introduction was not without disaster. In 1930, a laboratory in Lübeck, Germany contaminated the vaccines it was producing with a virulent strain of the tubercle bacteria, causing the deaths of over 70 vaccinated children.
Mistakes like the one in Lübeck became the impetus behind the development of biological safety cabinets and eventually, whole laboratories designed to safeguard lab workers and the general public from infection agents. Today, these laboratories are classified into four groups. Biosafety level 1 labs house biological agents that are dangerous but well-characterized and less likely to cause disease in healthy adults; level 2 labs handle agents with moderate risks; level 3 labs contain airborne agents that are considered potentially lethal; and those agents requiring the highest level of safety measures, biosafety 4, are both airborne and typically have no cure or treatment. Biosafety 4 labs require 10-pound full-body suits, multiple air locks, showers, and ultraviolet decontamination.
The recent anthrax shipment is just the latest in a history of hair-raising incidents. Here are a few more.

1971, Smallpox, Level 4:
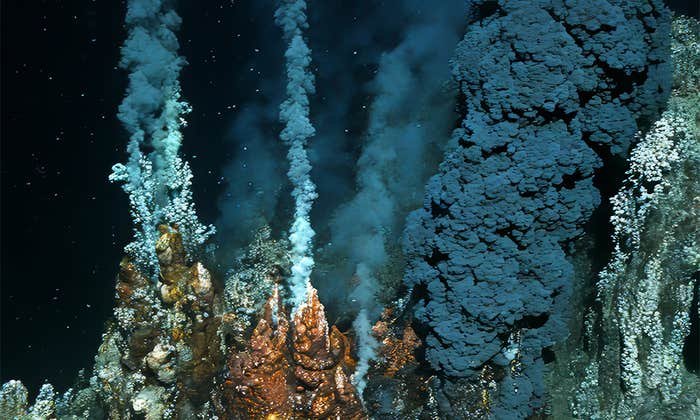
Near the center of the Aral Sea sits the island of Vozrozhdeniye, which housed a Russian biological laboratory and military weapons complex. In July 1971, remnants from the explosion of a smallpox weapon on the island traveled by air to a lab technician on the deck of a nearby research vessel, which was collecting plankton samples. By the time she returned to her home in Aralsk, Kazakhstan, she was afflicted by fever, headache, and muscle aches. She broke out in a rash, and her brother fell ill before doctors discovered it was a case of smallpox. Officials ordered mass vaccinations in Aralsk, then a city of 50,000, and hundreds of people were isolated in a special facility. Ten people were infected and three people would die.

1979, Anthrax, Level 4:
In April of 1979, something was killing the people of Sverdlovsk. Ninety-six individuals were infected with flu-like symptoms, and 64 of them died. For years after the outbreak, Soviet officials proclaimed the mass infection was due to a case of rotten meat. But a team of independent researchers investigating the outbreak in 1992 found that a nearby biological warfare base had accidentally released active anthrax spores into the air. In order to contain the epidemic, medical officials visited the homes of the infected citizens and dispensed antibiotics, stray dogs were shot, and local firemen washed the buildings and trees of affected neighborhoods.

1994, Sabia, Level 3:
In August of 1994, Sabia was a little known virus, having only been discovered the year before on a Navajo reservation in New Mexico. Like the other members of its family, it can cause headaches, muscle aches, vomiting, and internal bleeding. In late 1994, Dr. Jean-Paul Gonzalez was working with the virus in a test tube, wearing just a lab coat, a facemask, and gloves in a biosafety level 3 lab at Yale University. Then the test tube broke while spinning in a centrifuge, hurling its contents into the air. Following procedure, Gonzalez decontaminated the spill and hopped into a shower, dousing himself with a bleach-like solution. But he was alone in the lab at the time and did not report the incident. Even when he developed a fever a week later, he waited four more days before entering a hospital. By that time, he had exposed colleagues, friends, and family. He would go on to expose 139 people before being released.


2003, SARS, Level 4:
In July of 2003, the SARS outbreak that had infected over 8,000 individuals and killed almost 800 worldwide was finally brought under control. Five months later, a medical researcher at the National Defense Medical Center, which is affiliated with the National Defense University, in Taipei, Taiwan was working with the virus in a closed biosafety cabinet, through attached gloves. The waste of his research was being deposited into an attached compartment that contained a sterilization unit. Noticing spillage at the bottom of the attached chamber, and unable to reach and clean the spot with the attached gloves, Lieutenant Colonel Chan sprayed the area with alcohol and waited 10 minutes for any viruses in the spill to die. He then opened the chamber and manually cleaned the waste. Unfortunately, the virus survived, and he was infected. The next day, he flew on a plane and attended a conference in Singapore. Over the course of his travels, he encountered at least 90 people. A couple of days later, he developed a fever; and a week later, tested positive for SARS.

2014, Burkholderia pseudomallei, Level 3:
The Tulane National Primate Research Center hosts a high-security biosafety 3 lab. In November, non-human primates in the habitat section of the center were somehow infected by bacterial agents from the lab. The break was most likely the result of lax laboratory procedures, which did not mandate the removal of contaminated clothing before workers exited the lab. The bacterial strain that reached the animals, Burkholderia pseudomallei, is behind the disease Melioidosis, which can cause symptoms similar to tuberculosis or pneumonia. Researchers euthanized infected primates. But because B. pseudomallei thrives in soil and water, officials fear mass contamination of the primate habitat and the surrounding area, which is full of wetlands and moist terrain. The risk of illness to visitors of the area remains today.