For Macbeth, it was the ghost of his friend Banquo, sitting in a chair at the dinner table. In Edgar Allan Poe’s The Tell-Tale Heart, it was a disembodied thump-thump beneath the floorboards.
Guilt: It’s the emotion that arises when we know we’ve done another wrong. It’s an intrusive guest that can strangle us with regret and unravel the psyche. It feels larger than the body—which is perhaps why in fiction, it’s so often externalized to phantoms. Guilt tends to haunt people. It’s hard to expunge because the wrong deeds can’t be undone.
“As long as it’s plausible, it works.”
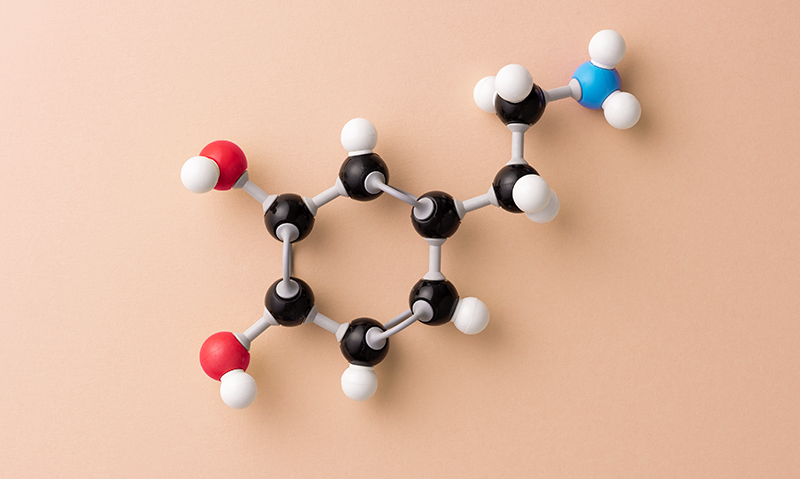
And yet researchers recently used a pill to reduce guilt in healthy human research subjects. In a study published in Scientific Reports at the end of last year, more than 100 people sat down for a “guilt induction.”1 They intentionally generated feelings of guilt by writing down a time they hurt someone they cared about. The researchers instructed participants to choose events that still made them feel bad when excavated from memory. Subjects later underwent a “guilt boost” where they were asked to close their eyes and dwell on the incident.
The purpose of the exercise was not to make study subjects feel bad, but to see if a pill could ease those bad feelings. The twist: The pill was a form of deception. It contained only lactose, sucrose, and glucose; it was a placebo. In the end, the study subjects’ feelings of guilt were significantly reduced after taking the pill—the pain of old hurts softened, the ghosts quelled.
The placebo effect is well documented. It’s a healing response to treatments that have no active ingredient, often delivered in a specific social and therapeutic context. Gold standard clinical trials have long sought to separate out placebo effects from effective treatments, precisely because the placebo effects are so real. But in the past couple of decades, researchers have sought to harness the power of the placebo effect as a treatment in its own right. Sham treatments, they have found, can alleviate a range of clinical conditions, particularly ones that have subjective and neurobiological components, such as fatigue, chronic pain, irritable bowel syndrome, and Parkinson’s disease.
Lately, the study of placebos has expanded to a more nebulous target: our emotions. They have been tested on a spectrum of distressing feelings, from guilt to anxiety, rumination, sadness, fear, and disgust.2 These emotions all play important roles in helping us process cues from our environment, learn from experience and move through the world successfully, but they can also become unmanageable, and when too persistent or intense, may lead to psychiatric illness, including depression and post-traumatic stress disorder.
More than 25 studies now offer evidence that placebos can regulate mild and acute emotional pain, with medium to large effect sizes, in both healthy and clinical populations, a review from this year noted. Placebos have been shown to reduce sadness in clinically depressed subjects who were watching sad movie clips or remembering upsetting memories, reduce the fear of public speaking in people diagnosed with social phobia, and lessen the fear of being shocked. A placebo nasal spray was also able to help people going through a break up feel fewer negative emotions when they saw pictures of their exes.
“I was obsessed with trying to help people regulate their emotions, but in a very easy way,” says Darwin Guevarra, a postdoctoral scholar at the University of California, San Francisco, and first author of the review. Emotions may arise in us easily, but they are hard to control, Guevarra says. It’s no simple task to “stop” feeling something on your own. Some of the strategies psychologists tend to recommend, such as cognitive reappraisal or mindfulness, can take a lot of practice and effort.
What makes taking a placebo easier than calming yourself down or working through a bout of sadness or guilt on your own? This is how Guevarra thinks of it: Placebos outsource emotional regulation onto placebo objects, like the pills or sprays commonly used in studies.
“If you’re outsourcing something, presumably it’s easier than if you were engaging in some strategy on your own,” Guevarra said. One consistent finding is that placebos seem to require less mental effort, compared to other emotional regulation strategies. Studies show they don’t interfere with other cognitive processes, suggesting that the effect may happen automatically, beneath the level of consciousness. In one study, people given a placebo while engaged in a working memory task—recalling a series of letters presented to them visually—still reported a decrease in pain following exposure to painful heat.3
In mental healthcare settings, where we typically wrestle with our emotions, some treatments are derided as working only through placebo effects. Calling a medicine a placebo is typically meant to suggest it’s a sham—but as researchers turn this idea on its head, they have uncovered some common features of placebo effects associated with certain therapies. These tend to include expectations, learned associations, a patient-clinician relationship, and a healing setting. Expectations are typically elicited through verbal suggestion, while learned associations may entail automatic responses to a familiar context or procedure.
“I came to the conclusion that you cannot separate placebo and psychotherapy,” says Jens Gaab, a clinical psychologist at the University of Basel, and the senior author of the guilt study. In psychotherapy, the patient-clinician relationship and healing setting lead many patients to expect relief, so long as the therapy proposed is believable. “It’s a contextual understanding,” said Gaab. “As long as it’s plausible, it works.”
Healing effects can occur even when subjects know that they are getting a placebo.
In one experiment, Gaab and his colleagues set out to show that even a bogus ritual could have a therapeutic effect. The researchers had three groups of healthy people watch videos of moving green circles, some of which changed colors.4 In one placebo group, people were told by a friendly, trustworthy, and empathetic researcher that the videos had a physiological impact that activated “early conditioned emotional schemata through the color green.” In the other two groups, people were told either that the video was being used to pass time or were paired with a non-empathic researcher. Only the group that received both a convincing rationale and interacted with an empathic researcher showed improvements in self-reported mood and stress.
“It was a fake idea, a fake rationale behind it,” Gaab said. “And it worked, people loved it.” It worked as well as a group psychotherapy treatment Gaab and his colleagues used with study subjects a few years earlier.
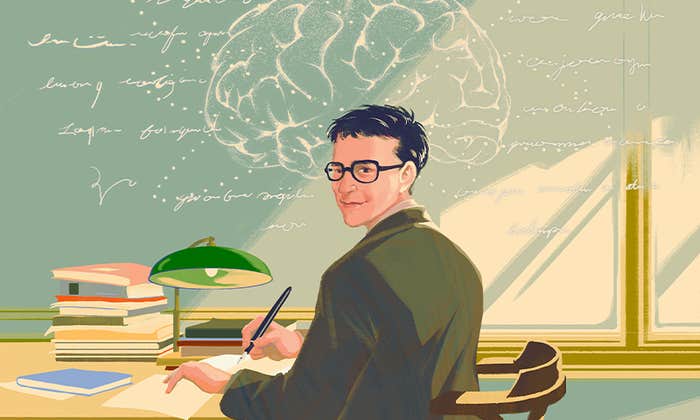
Imaging and pharmacological studies suggest that placebos work because the expectation of relief hijacks natural healing and reward processes in the brain,5 leading to the release of endogenous opioids and dopamine.6 These neurotransmitters are heavily involved in analgesia, reward and stress responsiveness, emotional regulation, and hedonic responses to food and social interactions.
According to one of the most prolific researchers in the field of placebos, Harvard professor of medicine Ted Kaptchuk, the placebo effect may be best explained by a popular theory of consciousness called “predictive processing,” or the “Bayesian brain.”
According to this way of thinking, the brain doesn’t just take in sensory signals from the body and the outside world and process them directly. Instead minute-to-minute perception consists of a series of best guesses, or predictions about the world, calibrated via a complex computation of values from sensory inputs, past experiences and subtle contextual cues. These predictions are constantly updated as new information comes in, and they can be heavily influenced by expectations and associations. Our bodies may then begin to respond as if what we have predicted were already true.
In one of the earliest writings about the placebo effect, a 1955 monograph in the Journal of the American Medical Association titled “The Powerful Placebo,” physician Henry Beecher wrote that patients needed to be in the dark about the fact that they got a placebo for it to work. He believed the duplicity was part of the magic. This view played a critical role in the application of placebos to medical research, where the most rigorous trial design is not just placebo-controlled but “double-blind”—the assumption being that even the clinician delivering a therapy could communicate subtle cues to a patient about whether it was real or fake that might influence its success.
But over the past decade, this fundamental assumption about how placebos work has been upended: Healing effects can occur even when subjects know that they are getting a placebo—that the treatment they are receiving has no active ingredients. These are called “honest” or open-label placebos, and the study of how and when they work has recently taken off.
In the guilt study, for instance, some people knew the pill was a sham, while others were told it contained a combination of herbs with psychoactive properties that could alleviate guilt. Shockingly, the pill worked to alleviate guilt whether they knew what was actually in it or not.
When and how much is it okay to lie to study subjects and patients?
“You would think this sounds ridiculous to tell people: You will get a pill or a natural spray, and there’s just nothing inside,” says Michael Schaefer, a professor of neuropsychology at Medical School Berlin. “But let’s see, maybe it will work for you, because some research has shown this. And indeed, people show effects.”
Researchers studying honest placebos want to understand not just how they work, but also get around an ethical quandary posed by deceptive ones: When and how much is it okay to lie to study subjects and patients?
In honest placebo studies, patients are typically educated about the placebo effect through a standard script—they learn that it can lead to healing outcomes in some contexts, that they work through expectation and previous conditioning, and that positive expectations can help but are not essential. In fact, the role of expectation in the success of open placebos is unclear. One study of placebos for irritable bowel syndrome from 2021 found that while high expectations led to better outcomes when deceptive placebos were used, low expectations were actually linked to greater symptom relief with honest placebos.7
Whether open placebos work as well as deceptive ones is still being explored. A review on open label placebos from 2021 found a significant overall effect on conditions like back pain, cancer-related fatigue, allergic rhinitis, irritable bowel syndrome, and menopausal hot flashes.8 For emotions, in addition to the guilt study, emerging evidence suggests that open label placebos may work. People who took honest placebo pills for five days experienced less emotional distress and said they felt better and slept better than study subjects who took nothing. Honest placebo pills also helped students manage test anxiety. And research published this year from Gaab and his colleagues showed even taking imaginary pills could reduce test anxiety.9
But open placebos don’t always have a therapeutic effect. A study from 2020 that aimed to harness the placebo effect to reduce sadness in women with major depression found that deceptive placebos worked significantly better.10 The deceptive placebo was better at lowering sadness levels following a “sadness-inducing” mood manipulation, but the open placebo was still able to prevent an increase in sadness after the mood manipulation, compared to the group that got no treatment. Some studies have also found that deceptive placebos lead to higher heat-pain tolerance than open ones, and the placebo effect disappears entirely when administered openly for motion-induced nausea.
The rules of open label placebos still need to be clarified. How does the role of expectation change when you know you’re taking something, that is really nothing? Shafir says she would predict that open label placebos bear greater similarities to other forms of cognitive emotional regulation than to deceptive placebos. But no one has tried to compare the relative effects of open label placebos versus an individual’s own personal effort to regulate emotions.
“This is something that is really essential for understanding the mechanism,” she says.
When it comes to regulating our emotions, we might have greater success harnessing the power of the placebo effect if we break it up into its component parts—expectation and conditioning—rather than focusing on fake pills and sprays and creams. In a study from February in Scientific Reports, Shafir and her colleagues set out to see if they could enhance study subjects’ efforts at emotional regulation using the power of suggestion combined with conditioning, a variation on the open placebo.11
Study participants were instructed to use distraction techniques (thinking about writing letters or drawing shapes) to lessen their experience of pain while being shocked. One group was told how helpful distraction could be at reducing pain and was conditioned to make that association in a first round of tests. Their first effort to use the distraction method was combined with a lower voltage of electric shock. The control group participants were told that the distraction technique was ineffective and received more intense shocks when they reported attempting it. Later, when people in both groups were shocked with equal intensity, the group conditioned to expect weaker shocks said that distracting themselves helped them feel less pain compared to the control group.
These new findings related to conditioning extend the way we look at placebos, Shafir says. “Because if we can use what we’ve learned from the placebo literature to enhance people’s internal control, that opens a whole new world.”
The combination of expectation and conditioning could not only help us maximize the placebo effect, it could also reframe our understanding of what a placebo is: It’s not just an external intervention, but something that happens within us. “People really like that,” Gaab said. “They have this sense of: It was me.”
Could we one day administer placebos to ourselves? There are some good reasons to think self-administered open-label placebos might not work as well; interaction with another person seems to be a crucial component. But there are cases in which it might work.
Guevarra offers an example from his own life. Several years ago, he began pairing his morning coffee with the application of essential oils to his wrists, creating an association between the effects of the caffeine and the smell. “Whenever I just activate the scent, it produces similar effects, just as caffeine would do,” Guevarra says.
Gaab thinks that as placebo studies progress, we’ll find that emotions are particularly sensitive to these effects. “Placebos work on suffering,” he says. “If people suffer, placebos can work.”
Other ethical conundrums may soon arise beyond whether it is ok to deceive someone into feeling better. For example, should the guilty be relieved of their guilt? Should the Lady Macbeths of the world not be wracked with remorse, condemned to smell the blood on their hands for all eternity?
Being able to regulate our emotions is adaptive, but our emotions are there for a reason. “Emotions are useful,” Guevarra says. “They are only problematic when they’re too long, too intense, when they’ve lost their usefulness. There are certain emotions that you should feel.” But maybe one day soon, it will be easier for any of us to dispatch the ones that have overstayed their welcome. ![]()
Lead image: Panimoni / Shutterstock
References
1. Sezer, D., Locher, C., & Gaab, J. Deceptive and open-label placebo effects in experimentally induced guilt: A randomized controlled trial in healthy subjects. Scientific Reports 12, 21219 (2022).
2. Guevarra, D.A., Kross, E., & Moser, J.S. Harnessing placebo effects to regulate emotions. PsyArXiv (2022).
3. Buhle, J.T., Stevens, B.L., Friedman, J.J., & Wager, T.D. Distraction and placebo: Two separate routes to pain control. Psychological Science 23, 246-253 (2012).
4. Gaab, J., Kossowsky, J., Ehlert, U., & Locher, C. Effects and components of placebos with a psychological treatment rationale—three randomized control studies. Scientific Reports 9, 1421 (2019).
5. Büchel, C., Geuter, S., Sprenger, C., & Eippert, F. Placebo analgesia: A predictive coding perspective. Neuron 81, 1223-1239 (2014).
6. Peciña, M. & Zubieta, J.-K. Molecular mechanisms of placebo responses in humans. Molecular Psychiatry 20, 416-423 (2015).
7. Lembo, A., et al. Open-label placebo vs double-blind placebo for irritable bowel syndrome: A randomized clinical trial. Pain 162, 2428-2435 (2021).
8. von Wernsdorff, M., Loef, M., Tuschen-Caffier, B., & Schmidt, S. Effects of open-label placebos in clinical trials: A systematic review and meta-analysis. Scientific Reports 11, 3855 (2021).
9. Buergler, S., et al. Imaginary pills and open-label placebos can reduce test anxiety by means of placebo mechanisms. Scientific Reports 13, 2624 (2023).
10. Haas, J.W., Rief, W., Glombiewski, J.A., Winkler, A., & Doering, B.K. Expectation-induced placebo effect on acute sadness in women with major depression: An experimental investigation. Journal of Affective Disorders 274, 920-928 (2020).
11. Shafir, R., Israel, M., & Colloca, L. Harnessing the placebo effect to enhance emotion regulation effectiveness and choice. Scientific Reports 13, 2373 (2023).