COVID has reached peak unsexiness. The thought occurs to me as I scroll through previously lively physician COVID forums where research, clinical quandaries, and professional anxieties were plentiful in March. Tonight, they are dormant. Even as the virus rages on. The moment of cutesy we-are-all-in-this-together GIFs, choral singing across Italian terraces, clapping for healthcare heroes has passed. Memes have moved on from kitsch and community-forming to shrill and preachy. Have we achieved psychological immunity?
I am a resident psychiatrist at Yale School of Medicine in New Haven, Connecticut. In March of 2020 I watched in astonishment and fear as the pandemic reached my state, the numbers of infected persons increasing in real time as our hospital scrambled to respond. Surgical and pediatric units were repurposed as COVID wards, calls for physicians to cross specialty lines were resounding. I donned recycled PPE and joined my internal medicine colleagues on the COVID medicine wards, calling upon my training from years prior to assist my overburdened colleagues. We treated those we could, applauding for them when they were discharged. We mourned those we couldn’t heal. In the psychiatric clinic—back at my day job—I faced patients with intensifying paranoia and hallucinations, new fantasies of suicide, recovery from opioid overdose. A new set of demons had been released into the air and for those already hanging on by a thread, it was too much to bear.
I once imagined the agony of illness being the greatest challenge I’d face as a doctor.
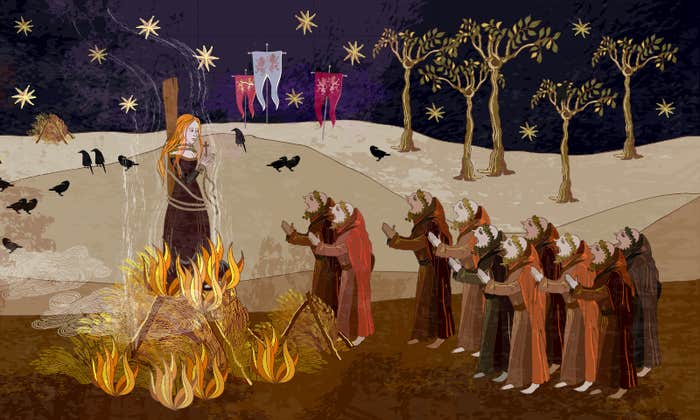
The moments I didn’t spend taking care of patients and worrying about my family, I dedicated to learning all I could about COVID—examining the emerging literature, relevant epidemiology, pathophysiology, and debating the evidence base—or lack thereof—for potential treatments with other physicians and scientists. While we were scared, we were energized, excited even. We believed that we could swoop in heroically and save our communities from wreckage by harnessing the lifesaving potential of science.
But we didn’t usher in salvation. COVID continues to flare, hitting new areas and reigniting those previously struck. Questions abound about reinfection, the trajectory of recovery, the durability of immunity. In our collective experience of illness, we oscillate between anxiety and a blend of complacency and fatigue. Medicine has a term for where we are right now: the chronic phase. A phase marked by tension between orienting around and orienting away from our illness. We worry about the effectiveness and tolerability of treatment and about symptom recurrence. But doubt creeps in too: are the preventative measures truly necessary for the long term? Are they too stringent? We fight against a pre-writing of a painful future and a rewriting of a pained past. I once imagined the agony of illness being the greatest challenge I’d face as a doctor. I learned that it is often the ache of chronic disease that stings most.
My most anxiety-provoking interactions with patients are during the chronic phase of illness. Residual symptoms linger, relapse, and treatment side effects loom large. Together we grapple with our limitations. I witness their reckoning with mortality, with the fragility of health and sanity. I wrestle with my inability to cure, with being unable to do anything to fix the problem. The weight of our vulnerability sinks in during the chronic phase. For patient and physician. No longer singularly focused on survival—preventing the suicide, obliterating the clot, stopping the hemorrhage—we confront the complexity of the bigger picture. There is no escaping the limits of our bodies, the limits of medicine, and the brokenness of social structures that make and keep people sick. The realities of racism, poverty, and structural inequality are splayed out before us in ugliness and in the relative uncomfortable calm of the chronic phase it becomes impossible to look away. The chronic phase compels us to commit to the long slog of battle.
Many of us become physicians because we are called to heal and we entertain fantasies of staving off illness, reducing suffering, preventing premature mortality. But treatment is seldom curative. And as indecent as it might be to acknowledge, ongoing management lacks the drama and excitement that often compel us. There are no TV series centered around the management of chronic back pain. Or diabetes. No crowd gathers to hear me tell the tale of the slow titration of Fluphenazine for my patient with schizophrenia. But my job isn’t to satisfy my own need to save. It is to heal. To sit with my patients and their pain, to tolerate the uncomfortable reality of their lives and suffering. Learning to embrace the not-knowing and the discomfort of bearing witness to the devastation that illness wreaks long after the drama fades has been a fundamental part of my maturation of a physician. The chronic phase of COVID is demanding of us that same maturation.
One cannot survive a chronic ailment without confronting one’s vulnerability. And a society cannot survive a plague without doing the same. Yes, we will learn more about this particular virus, a vaccine is likely to be developed but the fantasy that there will be an intervention that will tidily end our battle with COVID is fiction. Our vulnerability to global pandemics will remain as will the deeply entrenched injustices that create the environment in which they can thrive. There is no caped superhero on her way. Handwashing, mask-wearing and physical distancing are the easy part. The true challenge is to face the pain and suffering that exists all around us and know that doing so will not break us. It will enable us to repair what is broken. The cohesion and camaraderie that we relied on in the acute phase is needed now more than ever. The pain of chronicity is upon us. We will never be the same. And we mustn’t.
Ayala Danzig is a resident physician in psychiatry at the Yale School of Medicine. Follow her on Twitter @AyalaDanzig.