For the past three years, researchers at the Hubrecht Institute in the Netherlands have been painstakingly cataloging and mapping all the proliferating cells found in mouse hearts, looking for cardiac stem cells. The elusive cells should theoretically be able to repair damaged heart muscle, so the stakes in finding them have been high. Indeed, that search, involving many labs over decades, has been marked by heated debate and, recently, a call for the retraction of more than 30 papers for falsified data. This week, however, Proceedings of the National Academy of Sciences is scheduled to announce the results of the Hubrecht team’s work: no evidence of cardiac stem cells at all.
That conclusion, which confirms a long-standing suspicion among some in the field, cuts to the heart of a deeper question—about what it means to be a stem cell. As more sophisticated technology has revealed just how plastic and heterogeneous cell populations can be, some researchers have transitioned from viewing “stemness” as the defining trait of a cell category to viewing it as a function many types of cells can perform or contribute to.
Stem cells were first identified and characterized in bone marrow in the 1950s and ’60s, in an effort to understand and treat the consequences of radiation exposure after World War II. These blood stem cells were rare, slow to divide, and capable of both self-renewal and differentiation into any of the blood’s more specialized cell types. They maintained the body’s reservoirs of blood cells and helped it respond to damage. When they were irradiated, they died and the body had no way to replace them—but bone marrow transplants (which held stem cells) enabled the system to regenerate.
We have to be more accepting of the fact that, in principle, any cell can be a stem cell.
Because of their relevance to healing and recovery, stem cells in other tissues became coveted prizes among researchers and physicians searching for ways to treat all sorts of conditions and diseases.
Then the story got more complicated. Stem cells were identified in other adult tissues throughout the body: in the skin, in hair follicles, in the gut—and a few months ago, in bone. They, too, could self-renew and give rise to their tissue’s various cell lineages. But otherwise, they looked very different from the blood stem cells. They expressed different genes, exhibited different protein and surface markers, and divided in different ways and at different rates.
In the 1990s, scientists isolated embryonic stem cells, which were even more powerful than those in adult tissues, with the ability to become any cell type in the body. Around the same time, scientists began looking into the part that cancer stem cells might play in the growth of tumors. And in 2006, researchers succeeded in transforming differentiated connective tissue cells into induced pluripotent stem cells (iPSCs), which had the versatility of embryonic stem cells. That result showed that stemness could be induced.
Yet looming over these findings, according to the molecular geneticist Hans Clevers, an author on the new PNAS cardiac stem cell paper, is the assumption that stem cells throughout the body are “a precious, hard-wired, magical entity” like the ones in bone marrow. In fact, he said, those first insights gained from blood stem cells have colored how scientists think about stem cells in other tissues—sometimes in ways that have been profoundly limiting.
Many Routes to Tissue Repair
One often-overlooked point is that “many tissues can repair themselves in very ingenious ways,” Clevers said. “There is no set strategy.” In the blood, the small stem cell population is the only means of regeneration, but in solid tissues, that’s not always the case. The stem cells themselves are different: They tend to divide more rapidly, for instance, and because they exhibit unique molecular profiles, they have to be identified by methods specific to them. Reliance on tissue-specific markers (which aren’t always stringent) is one of the reasons there’s been so much debate surrounding whether cardiac stem cells exist—and why it remains so difficult to determine other types of stem cells.
Moreover, when the stem cells in solid tissues are destroyed, more specialized cells in those tissues can often revert to a stemlike state to take over repair functions on their behalf. Cells are therefore much more plastic than previously thought possible, with less fixed identities. “There’s more and more evidence saying that our bodies can respond to damage independent[ly] of what we would consider a classic stem cell population,” said Jonathan Hoggatt, a hematologist and stem cell researcher at Harvard Medical School and Massachusetts General Hospital.
That’s been shown in a slew of organs, including the kidney, lung, stomach, and intestine. Perhaps most striking, some tissues (beyond the heart) don’t seem to have a stem cell population. The adult liver—the epitome of efficient organ regeneration—has no stem cells; instead, its differentiated cells can act like stem cells when needed. “In essence,” Clevers said, “every cell in the liver has the potential to behave like a stem cell.”
And so, “it’s more useful to find out how a particular tissue performs its stem cell function than to identify individual stem cells,” he said. The way various cells all contribute to maintaining a tissue constitutes stemness—not any one cell type or entity. Sticking to the more dogmatic definition of what a “true” stem cell should be, instead of considering that they fall along a more nebulous spectrum, has hindered progress.
In fact, researchers have found that even those “true” stem cells vary in potency and behavior. “We’re learning there’s much more heterogeneity in what we thought were pretty homogeneous populations,” Hoggatt said.
Dubious Stem Cells, Phony Treatments
As it’s become increasingly difficult to distinguish stem cells from others that have already begun to commit to some differentiated cell fate, it may be necessary to revisit older research. Pamela Robey, a biologist at the National Institutes of Health who focuses on the skeletal system, thinks that the newly identified skeletal stem cells may actually be progenitor cells—the recent, slightly more differentiated offspring of stem cells—instead. The actual skeletal stem cells, she argues, are even more rare and still need to be identified. “It’s very easy to trick oneself into thinking that you have a true stem cell,” she said, “when that may not be the case.”
That’s sometimes led to controversies, most notably when it comes to what are known as mesenchymal stem cells—a diverse and multipotent category first extracted from bone marrow, though they don’t make blood cells. Currently, most researchers don’t consider them to be stem cells at all (and many have stopped calling them that), but a history of confusion about what they are and what they do has made them “ripe for exploitation,” Robey said. Unapproved stem cell clinics have taken advantage of their controversial status to treat thousands of people with ineffective, unproven, and potentially dangerous therapies. In reality, only a handful of stem cell treatments, using certifiable stem cells, are allowed by the Food and Drug Administration—and those all involve some version of bone marrow or blood cell transplant.
But for scientists who observe the proper regulations, a wider definition for stem cells could be good news for medicine: It means that regenerative treatments don’t need to target only populations of stem cells, which may not always exist. Rather, they could make use of more differentiated cells that fulfill some stemlike criteria. Some researchers have decided not to consider stemness as a factor at all when coming up with new pharmaceuticals involving living cells. “It makes life easier,” Clevers said.
Going forward, he added, “we have to be more open-minded, more accepting of the fact that in principle, any cell can be a stem cell.”
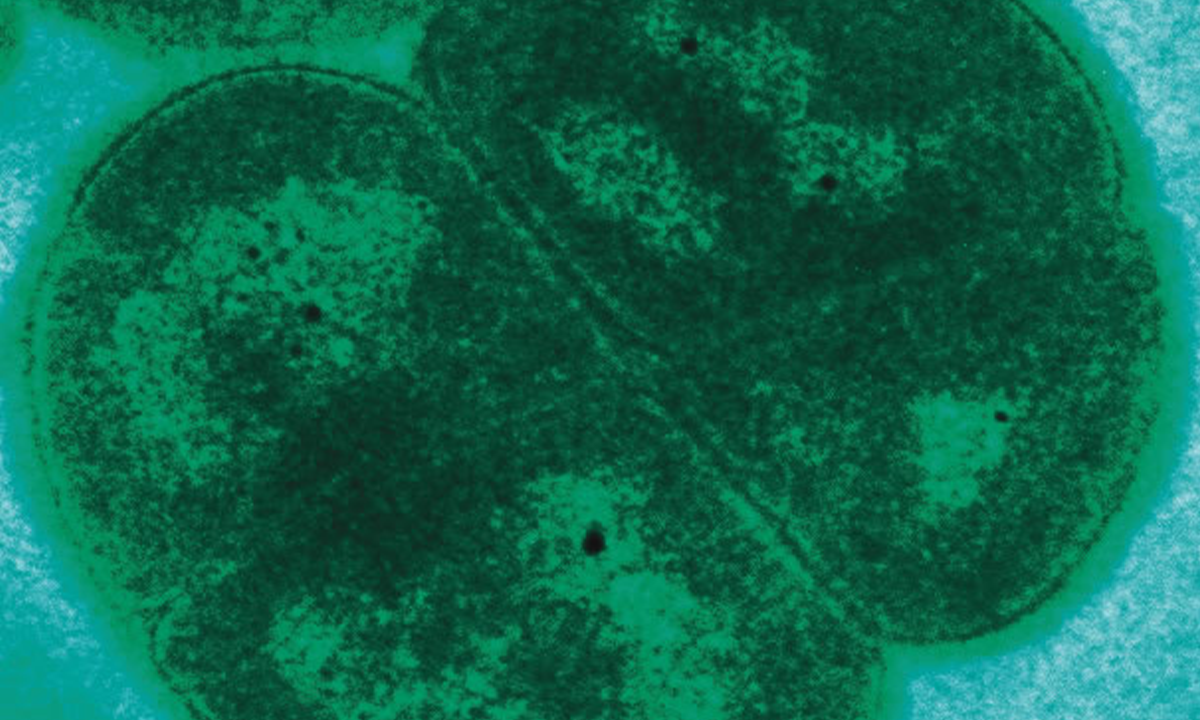
Lead image credit: Lucy Reading-Ikkanda/Quanta Magazine