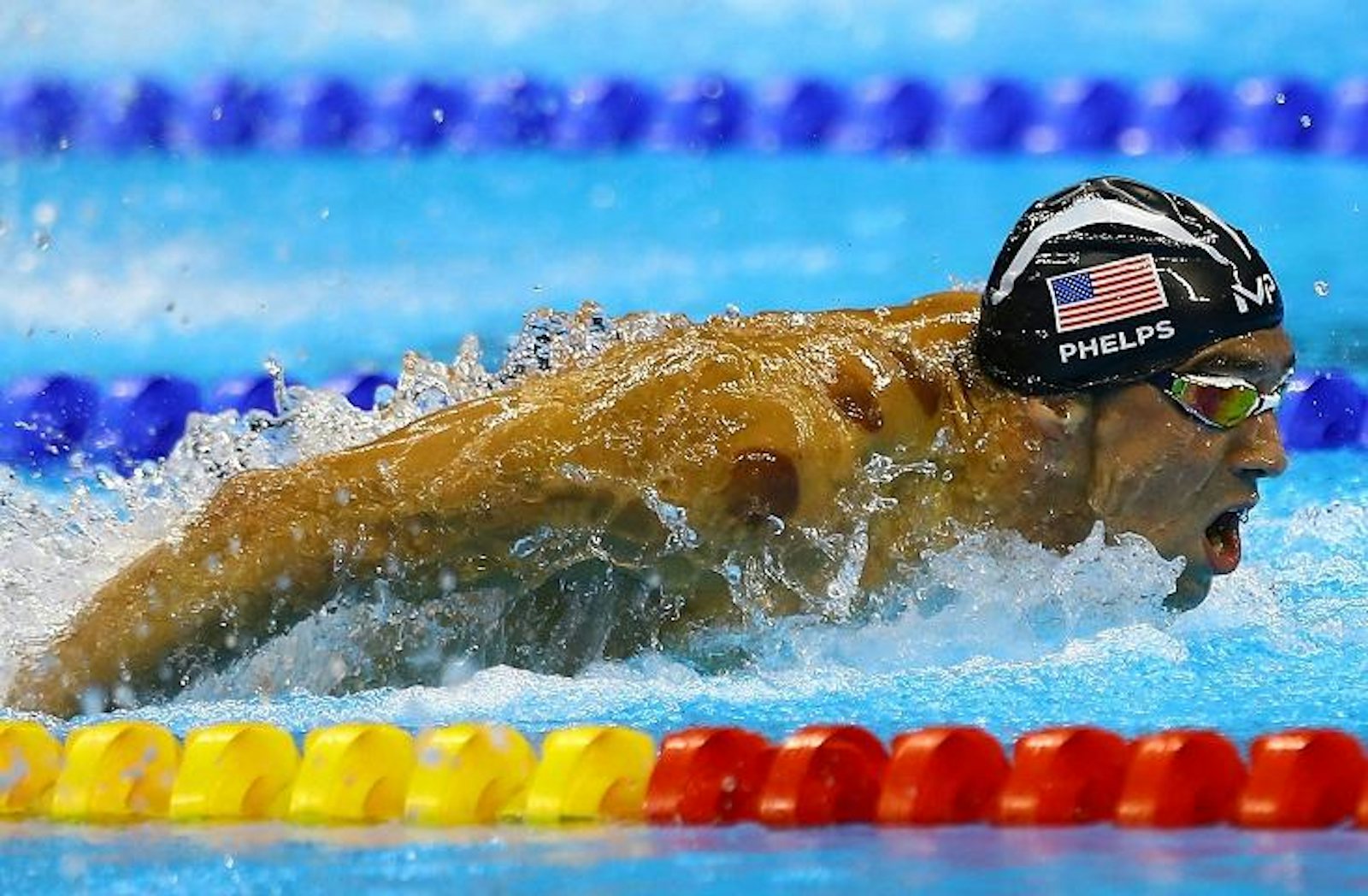
Several days ago, when the Rio Olympics began hitting their stride, many athletes, including champion swimmer Michael Phelps, were sporting a unique look: Their muscled shoulders were spattered with, well, what? Giant purple chicken pox? Alien hickeys? Soon enough, however, the marks were demystified: They were evidence of cupping, a therapy that involves placing suction cups on the skin, then using the suction to pull the skin up off the muscles (not unlike the pressure caused by giving someone a hickey.)

By applying localized pressure, the treatment is thought to increase blood circulation to the area it targets, relieving painful tension by increasing circulation, decreasing inflammation, and potentially releasing lactic acid buildup. Additionally, the increased inflammation triggers an immune response, causing a flood of small proteins called cytokines to enhance muscle repair.
While cupping has been used by athletes and alternative therapists for years, the media frenzy caused by the Rio Olympics has given the practice its 15 minutes, revealing it has a number of die-hard adherents, including celebrities Jennifer Aniston and, of course, Gwyneth Paltrow.
Romy Lauche, a research fellow at the Australian Research Center in Complementary and Integrative Medicine, explains that cupping in ancient medicine was “a kind of bloodletting, where the skin was punctured, and a cup, or a horn, or a bamboo vessel, was applied to the area, sucking out blood and other fluids.” Healers claimed it would detoxify the body.
Cupping has come a long way since then, and today the most common practice is dry cupping, which doesn’t puncture the skin. However, since cupping is not an FDA-approved treatment, it’s hard to say whether it actually works.
“Very few studies were performed to study the effects of cupping,” Leonid Kalichman tells Nautilus in an email. Kalichman is a senior lecturer in the physical therapy department at Ben-Gurion University of the Negev in Israel, and coauthor of the paper, “New is the Well-Forgotten Old: The Use of Dry Cupping in Musculoskeletal Medicine.”
While three randomized controlled trials have shown improvements thanks to cupping, these trials did not always show cupping’s effects as separate from other kinds of pain relief measures, such as progressive muscle relaxation. Its benefits may actually be largely placebo-based—some of cupping’s advocates note that the psychological impact of cupping could be just as powerful as its purported physiological ones. “We cannot rule out a placebo of such intervention. Cheap and safe placebo[s] also can be beneficial for athletes,” Kalichman says.
But, for a placebo, it may not be risk-free. Several studies have shown that cupping may actually be risky. That was the conclusion reached in a 2009 paper in Medical Hypotheses, called “Can traditional ‘cupping’ treatment cause a stroke?” by Stevia Blunt, a neuroscientist at Imperial College’s School of Medicine, and Heow Pueh Lee, a professor in the department of mechanical engineering at the National University of Singapore. Blunt and Lee presented the case of a 55-year-old man who, one evening, received a cupping treatment to his back and spine, and to the anterior triangle of the neck. The man reported discomfort during the experience. The next morning, around 14 hours after his treatment, he awoke with a constant, dull headache on the right side of his head. Around four hours later, the man realized he had started losing vision in his left visual field; over the next few hours, his left visual field became entirely occluded.
The man was examined, and found to have had a hemorrhagic stroke, in addition to left inferior quadrantanopia, or loss of vision in his left visual field.
When the researchers searched for existing conditions that may have led to the stroke, they found none. The man didn’t have preexisting hypertension or stenosis—conditions associated with hematoma and stroke. And his particular condition, primary intracerebral hemorrhage, usually results from an acute rise in blood pressure, which generally happens in the context of more sudden experiences of emotional stress, drug use, or physical pain—the latter of which the man had experienced in his procedure. In the weeks following the cupping procedure, with no additional procedures, his condition improved; the hematoma resolved itself.
Blunt and Lee concluded that the patient’s cupping treatment may have caused his blood pressure to rise by stimulating receptors in his blood vessels, resulting in intracerebral hemorrhage. Additionally (or alternatively), because he found the procedure painful, it could be that cupping overstimulated his nerve fibers, also leading to an acute rise in blood pressure. The researchers surmised “cupping of the cervical area may cause a hemorrhagic stroke,” and cautioned against applying a cupping treatment—which stresses blood vessels—to an area where those vessels may be already torn.
This latter finding is especially pertinent for athletes, whose daily exercises and strains cause constant, microscopic tears in their muscles. While these tears encourage extra protein synthesis—leading to the muscle growth we refer to as “body-building”—they could also put athletes at risk for hemorrhages associated with cupping, even while potentially enhancing the “good soreness” associated with a good workout.
Kalichman does remark that, while several studies have noted “complications” due to cupping, most of these involved therapists with less advanced training. Because athletes are healthier than most patients, and receive advanced care, they’re unlikely to experience the negative side effects that non-Olympians might have to face.
The risk of treatments is unlikely to be zero, however. Are the benefits worth it? Can cupping improve athletic performance? “It might help with muscle recovery due to increased circulation and reduce muscular pain,” says Lauche. “It is, however, not a miracle treatment, and I fear it will not improve athletes’ performance by and large.”
Susie Neilson is an editorial fellow at Nautilus.