Rosalinda Roberts had gotten used to seeing weird shapes in the brain. Over three decades of looking at brain tissue under an electron microscope, she’d regularly come across “unknown objects”—specks and blobs in her images that weren’t supposed to be there, and didn’t seem to relate to the synapses and structure that she was studying. “I’d just say, ‘well I’m not going to pay attention to that’ ” she explains. That’s all changed now.
Finding bacteria in the brain is usually very bad news. The brain is protected from the bacterial menagerie of the body by the blood-brain barrier, and is considered a sterile organ. When its borders are breached, things like encephalitis and meningitis can result. Which made it all the more surprising when Roberts, along with Charlene Farmer and Courtney Walker, realized that the unknown objects in their slides were bacteria.
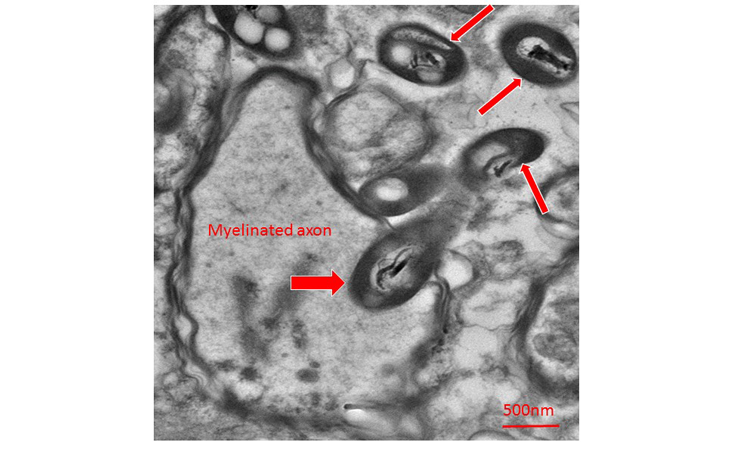
Many of them were caught mid-stride, entering neurons or penetrating axons. Others were in the process of dividing. They were picky, too, strongly preferring some regions of the brain over others. The surrounding brain tissue showed no signs of inflammation. If the bacteria were in the brain while the individual was alive, they were not pathogenic.
If it’s confirmed—contamination has not been definitively ruled out—the work opens up new avenues of research into the microbiome and disease. The group presented their results this month at the annual Society for Neuroscience meeting this month, and Nautilus caught up with Roberts last week.
Why do you think your images have caused so much excitement?
If there really is bacteria getting into the brain from the gut while an individual is alive, it’s a real paradigm shift because the brain has been, among other organs, considered sterile. To find bacteria there in non-traumatic, non-infectious samples is just completely unexpected.
How did this line of research begin?
I’ve studied schizophrenia for virtually my whole professional career. I do that by looking at synaptic differences and pathology that might be present in schizophrenic post-mortem brains. Over the years I would see these unknown objects, and disregard them. Then I had an undergraduate student who was part of an honors program here at the University of Alabama, Courtney Walker. She was studying the substantia nigra, which is a region of the brain that contains dopamine neurons. She kept seeing these objects—we called them “those things”—and kept poking at the problem. It started to become a lab obsession.
How did you learn the mystery objects were bacteria?
Based on morphological criteria, I began to suspect that they were bacteria. I showed the pictures to a bacteriologist and he said, “those are bacteria.” Then we went on to do a ribosomal analysis and found that they were gut bacteria, which is very interesting because of the interest in gut-brain work these days.
The bacteria might enter the brain through the blood-brain barrier. There are places where it’s not that tight.
What do we know about gut-brain behavior?
You can manipulate behavior and cognition and even structure with the microbiome. If you take germ-free mice, which have no microbiome, and colonize them with regular mice feces using a fecal transplant, a lot of their behavioral symptoms will become ameliorated. And if you put H. pylori bacteria into mice, they develop new cognitive and behavioral problems. The fecal microbiota (which is the gut microbiota obtained from feces) is different in people with different illnesses. People with Parkinson ’s have a different microbiota than people who don’t have it.
What have been some of the proposed mechanisms describing how the microbiome influences the brain?
You know, I haven’t seen one. Whatever speculation there has been, has been on the route by which information gets up to the brain. One speculation is that it travels up through the nerves that innervate the stomach. One of them is called the vagus nerve. There’s one study where scientists severed the vagus nerve, and they could no longer manipulate brain behavior by altering the microbiome. That suggested whatever they were doing was going up the vagus nerve, but what that was, they never said.
If bacteria do physically travel from the gut to the brain, how might they get there?
I’m not a microbiologist, so take my speculation as such. If the bacteria goes up the vagus nerve into the brain, it would have to just burrow into the myelin and go up through interior transport, I suppose, to get up to the dorsal nucleus, and then leave and go elsewhere in the brain. The bacteria might also enter the brain through the blood-brain barrier. There are places in the brain where it’s not that tight. One of those areas is called the chemo-sensitive trigger zone. It’s in the brain stem, and it’s a place where the blood-brain barrier is full of holes. The reason for this is that the brain needs to know if you’ve eaten something toxic so it can provoke vomiting. The blood-brain barrier around the pituitary isn’t very tight for similar reasons. I want to look more closely at areas where the blood-brain barrier has a lot of holes, to see there are more bacteria there.
Did the bacteria you saw prefer some parts of the brain over others?
We saw that they like to be inside astrocyte cells around the blood-brain barrier. They also like to be in axons, which are projections between brain regions that conduct information. Axons are covered in myelin, which is a fatty deposit. Additionally, in mice but not in humans, the bacteria like to go into the nucleus of neurons. It’s very unclear what this means. Why would they prefer to invade certain cell types? I know that certain types of bacteria like fat, and others like sugar. The myelin is fatty and the astrocytes have sugar. The distribution of bacteria also suggests that our observations are not entirely due to contamination, or we’d see the bacteria everywhere, not just in particular regions.
Could this just be bacteria entering the brain after death?
That was what I first thought—maybe this is bacteria invading and starting to munch up the brain. But they were also seen in mice brains fixed immediately at death, without any postmortem artifact or any length of time for bacteria to invade. So it’s not a postmortem artifact of postmortem decay kind of thing. Also, at the time of processing, the brain is either put into a fixative, or frozen. I’m at a loss to explain how bacteria would be able to enter the brain after processing. Why would they go into a brain that’s fixed in a hostile, anti-bacterial solution?
Dead bacteria sort of looks like ghosts, just fragmented cellular morphology. These don’t look like that.
Can you rule out some other form of contamination?
I cannot rule out contamination at this point. But even if it is contamination, the bacteria are very, very particularly distributed. They’re not just a wash all over everything. They gravitate to certain intercellular compartments, which is very interesting in itself. We have to rule out contamination with a very systematic study, with everything sterilized and autoclaved, and process germ-free mice and regular mice, and human brain samples.
Did the brains you looked at show any signs of inflammation due to the bacteria?
The bacteria don’t seem to provoke an inflammatory response, which is peculiar because you think they would. That suggests either the whole thing is postmortem or post-fixing contamination, or that they’re just not pathogenic to the brain.
Are the bacteria alive?
I think they are alive. They certainly look healthy. Dead bacteria sort of looks like ghosts, just fragmented cellular morphology. These don’t look like that. It would be most interesting if they were alive, and frozen in time in the postmortem brain. I’d like to see if I can culture the bacteria I see, to see if they’re really alive, then do some experiments to try to gain some insight into why they like different areas of the brain. The 16S microbiome analysis we performed doesn’t tell you how many bacteria there were, or if they were alive.
Do you see any dead bacteria?
I don’t see dead ones. They would be munched up by macrophages in the usual way, or processed through the lysosome pathway. The ones I see are structurally intact and many of them have septum in them, which suggests that they’re dividing.
Another control you used was brains from germ-free mice. What did you see?
We looked at four germ-free brains. Two of them we examined with electron microscopy, and we didn’t see any bacteria. Two of them we examined with a 16S microbiome analysis, which showed them as having bacteria. But the microbiome analysis doesn’t tell you how many bacteria there are, it only tells you the proportion of different bacteria in a given sample. So you could have 0.0001 grams of bacteria in the germ-free mouse and 150 grams in a wild-type mouse and the microbiome analysis wouldn’t reflect that. You can get snippets of bacteria that have been killed in the food showing up in the 16S analysis. And we also need to measure the reagents used in the 16S to see if any of the reagents are introducing bacteria.
What else do you want to try?
One of the approaches that was suggested to me was to transplant labeled bacteria into germ-free mice, and see how long it took for them to get to the brain. I’d also like to look at my postmortem collection, and see if different diseases change either the location of bacteria in the brain, or the type of bacteria. It’s interesting that I did not see any H. pylori in the brain. That’s a type of bacteria that people are saying can cause cognitive impairments.
Why present this research in a poster?
I needed to see what the scientific community thinks about it. I wanted to see if I could hook up with some microbiologists or other people who might be studying this in ways that it’s just hard for me to do. And that resulted in just that. I’ve gotten calls from scientists saying, “Hey, let’s exchange papers and talk about this.” It takes so long to get a paper published that by the time it’s published, you’re onto something else already. So this is a format where you can show your preliminary work, talk to colleagues about what they think, and discuss where you’re going with it, rather than just sitting in your office scratching your head wondering, “What is this?”
Why do you think your lab was the one to make this discovery?
There’s not that many electron microscopists left in the world. Neuroscientists now want to be molecular, intracellular, mechanistic, and more well-rounded. Human postmortem electron microscopy is very rarely done. There’s only really one other group that does it. It’s a matter of getting electron microscopists hooked up with a brain bank or a collection that has tissue with very, very short postmortem intervals. And that combo doesn’t usually occur together.
The Alabama Brain Collection, which you head, sounds like a big asset for this research.
Yes it is, but let me put a caveat on it. For electron microscopy, you need to have the brain processed within eight hours of death. The average postmortem interval is closer to 24 or 30 hours. So it could be there’s only 10 or 15 percent of the subjects that I have that are actually suitable for electron microscopy.
Michael Segal is Nautilus’ editor in chief.






























