Back in 2000, before MRSA—Methicillin-resistant Staphylococcus aureus—had become a household word, Nobel Laureate Joshua Lederberg wrote in the journal Science that “the future of humanity and microbes [would] likely unfold as episodes of a suspense thriller that could be titled Our Wits Versus Their Genes.” Thirteen years later, it is “their genes” that seem to be winning out. In the United States alone, roughly 2 million people suffer from drug-resistant infections each year; according to the most recent Centers for Disease Control and Prevention (CDC) report, about 23,000 of them die.
While the microbes have cracked almost all of our codes—rapidly evolving around one drug after another—we have yet to fully crack many of theirs. Scientists have a growing understanding of the molecular wizardry by which bacteria develop resistance to antibiotics, but they have yet to circumvent it. In the meantime, doctors and patients are forced to fight these drug-resistant infections with alternatives that harken back to the medical stone age (think toxic chemicals and surgical removal of whole organs to stop bacterial infections). And even those solutions are failing.
Ten years ago, experts worried about our eventual return to the pre-antibiotic era of medicine, when common bacterial infections were the stuff of life and death. Today, scientists say that return is now upon us. “We’re on the brink of a medical catastrophe,” Dr. Thomas G. Slama said in a 2012 press release, when he was president of the Infectious Diseases Society of America.
If we could observe that brink through the lens of a high-powered microscope, we’d see the latest round of a molecular code-based war that humans and microbes have been fighting for as long as both have occupied the same planet. But while we may be losing the battle, we may still win the war. Our latest salvo is a clever one, exploiting a genetic code called CRISPR that is tucked into the bacteria’s own genome.
Antibiotics are, by far, the greatest weapon we humans have had in this contest. Most of them work by interfering with the production of proteins and other molecules that are crucial for bacteria—for their function, metabolism, or replication—but play no role in human cells. For example, Penicillin impedes the cross-linking of peptidoglycan, a polymer that bacteria use to build their cell walls. When the units of peptidoglycan can’t link together, the bacteria end up with very fragile walls, which easily break open, causing death. It’s a neat trick because human bodies don’t need peptidoglycan to function, so antibiotics can kill the microbes without killing us. Ciprofloxacin, an antibiotic used to treat everything from urinary tract infections to anthrax, blocks the enzyme that enables bacterial DNA to coil and uncoil as needed.
But bacteria are experts at survival. When a bacterium is under stress, for example when it is exposed to antibiotic drugs, it snatches up whatever bits of genetic material it can grab from its external environment. It does this mainly by picking up plasmid DNA—autonomous DNA molecules which carry only a few genes—from other bacteria, including those of vastly different species, and even those that have died. The process, known as horizontal gene transfer, occurs through bacteria’s cell walls and is much faster than human evolution, which takes place gradually over many generations. It enables bacteria to acquire whole genes in one exchange, and to pass those genes on to its neighbors with remarkable speed and efficiency. In the human-microbe war, horizontal gene transfer is the equivalent of intelligence sharing between allies. Bacteria exchange secret codes through which they conspire to overthrow us.
“Under hostile conditions, they start incorporating whatever genes they can find into their chromosomes in the hopes that one of those genes will give them an advantage,” says Luciano Marraffini, a microbiologist at The Rockefeller University on Manhattan’s east side.
Bacteria exchange secret codes through which they conspire to overthrow us.
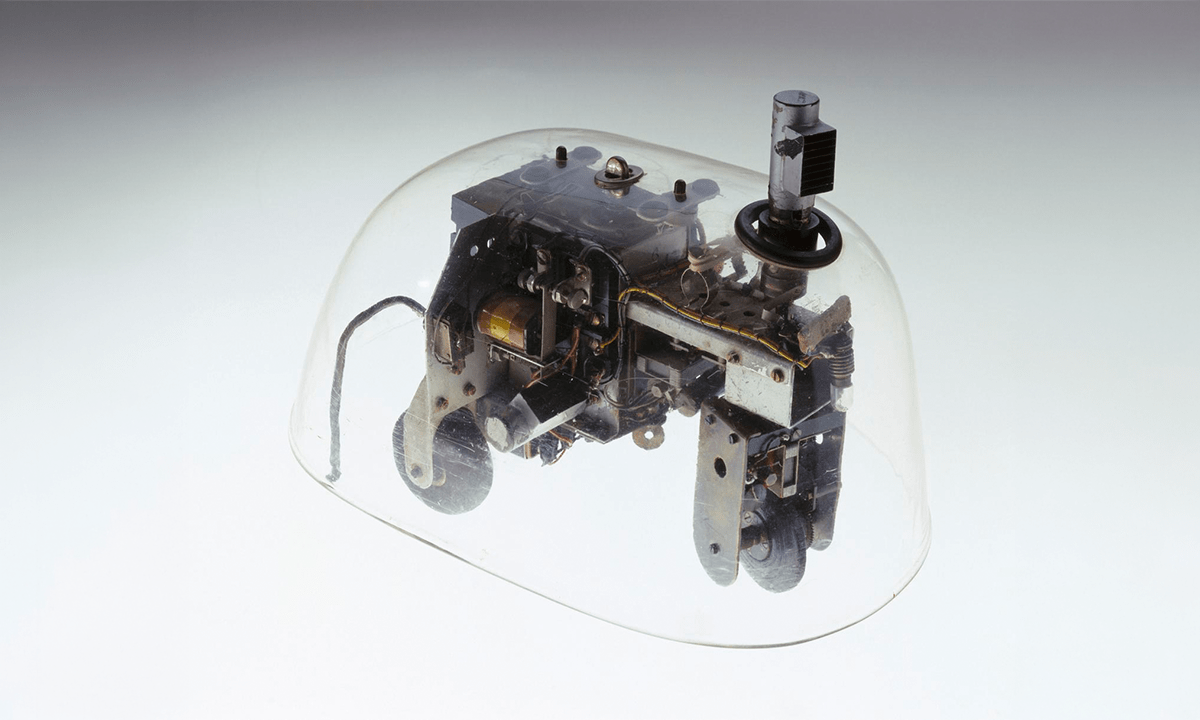
It turns out that while they lay waste to us humans, bacteria are also fighting another battle, against viruses called bacteriophages—or phages for short—that would otherwise lay waste to them. And as they challenge our immunity, they fight off phages with a cryptic and powerful immune system of their own.
When Marraffini was still a graduate student at the University of Chicago, Rodolphe Barrangou, a food scientist at North Carolina State University, made the first major breakthrough into what purpose the CRISPR code serves. The paper explained that CRISPR, which stands for Clustered Regularly Interspaced Short Palindromic Repeats, is a distinctive genome feature of many bacterial species which they use to fight phages. Scientists had already determined that some bacteria possessed long stretches of repeating DNA sequences, but had no proof as to what purpose these sequences served.
Barrangou showed that each time bacteria are invaded by a phage virus, they claim a snippet of that virus’s DNA and incorporate it into their own genome. But they don’t stick that viral DNA just anywhere; they tuck it into the CRISPR sequences, so that the palindromic repeats are interspersed with non-repeating “spacers” of phage DNA. The spacer sequences then serve as a memory of past phage infections, essentially functioning as a bacterial immune system. When the bacteria are attacked again by the same virus, they match the invader DNA to the spacer DNA. This identification then sets in motion a molecular machine that ultimately tears the phage virus to shreds.
Marraffini, who at the time was studying spore-formation in Bacillus anthracis (the process by which this anthrax-causing bacteria forms the tough protective spores that enable them to survive for decades) was captivated by Barrangou’s findings. He began studying the phenomenon in his spare time, looking at CRISPR systems in Staphylococcus epidermidis.
It took him about a year to make a discovery of his own, one with huge implications for antibiotic resistance. It turned out that not all CRISPR sequences contained phage DNA. Some of them, in fact, many of them, contained plasmid DNA from other bacteria. This meant that the CRISPR destroying system works against all forms of foreign DNA—it assimilates gene snippets that originate both from viruses and other bacteria. A positive identification of a phage or bacterial plasmid would destroy either one, together with the genes it carried.
Each time bacteria are invaded by a phage virus, they claim a snippet of that virus’s DNA and incorporate it into their own genome.
Marraffini wondered what would happen if CRISPR incorporated some beneficial genes into its seek-and-destroy list—even if by accident. Would it then detect and eliminate plasmids carrying such genes? It would prevent bacteria from incorporating antibiotic resistance genes into the genome and passing them on to future generations, which would be against the bacteria’s own best interests, but like any other system, the CRISPR code could have a glitch.
To test this hypothesis, Marraffini injected a mouse with two different versions of pneumococci, the bacteria that cause pneumonia. The first injection contained a live but avirulent strain of pneumococci, which didn’t have a gene that codes for the sugar capsule that normally encases pneumococci and enables them to slip into and infect a host cell. That avirulent strain also contained a CRISPR sequence that held snippets of that gene. Then Marraffini injected the same mouse with heat-killed pneumococci that still possessed the sugar capsule gene.
Normally the live avirulent pneumococci would have saddled up to its dead cousins and grabbed the capsule genes through their walls. Then they would have used those genes to make the capsule, transform themselves into a virulent strain, and proceed to infect the mice with deadly pneumonia. Marraffini’s mice should’ve been dead soon after injection. But days later, they were perfectly healthy. The CRISPR system had prevented the plasmid carrying the capsule gene from being transferred between the two bacterial strains or destroyed it upon arrival. And without that gene, the live bacteria hadn’t been able to invade the mice’s lungs.
It looked like the CRISPR code did indeed have a loophole that could prevent infectious bacteria from acquiring antibiotic resistance genes. Marraffini describes it as a byproduct of how the system evolved. If CRISPR were to incorporate genes coding for antibiotic resistance, bacteria could essentially be turned against themselves. And scientists would turn the tide against one of humanity’s greatest modern scourges.
Marraffini’s findings made a splash in the scientific community. When his first CRISPR study was published in the journal Science in 2008, Marraffini had barely begun his post-doctoral fellowship; but by 2010, he had secured his own lab at The Rockefeller University in Manhattan. And by 2012, he had won the New Innovator Award, a prestigious and competitive grant from the National Institutes of Health.
It looked like the CRISPR code did indeed have a loophole that could prevent infectious bacteria from acquiring antibiotic resistance genes.
Since CRISPR behaves this way both in the lab and in nature, Marraffini’s research raises an interesting question: How can bacteria possess a defensive system that, when manipulated, as in Marraffini’s study, will destroy the plasmid carrying the same antibiotic resistance genes it routinely manages to acquire, use, and pass on? So far, the answer seems to be that they can’t. Several studies have found a negative correlation between the presence of CRISPR and the presence of antibiotic resistance genes. In other words, a given bacteria can have one or the other, but not both.
Marraffini thinks bacteria have the ability to somehow rid themselves of CRISPR when the situation calls for it. “The bacteria make use of CRISPR when confronted with a phage, and then shut down CRISPR when they need to try and acquire antibiotic resistance genes,” he says. “It should be possible to disrupt that cycle at various points, or even to turn it against the bacteria.”
Designing CRISPR sequences that block specific genes—as Marraffini did in his mouse study—is easy enough. “It’s basic molecular biology to target a gene sequence and insert it into a bacterial genome,” Marraffini says. “And you can insert as many gene slices as you want into CRISPR.” But getting those CRISPR sequences into the bacteria while they’re attacking a human being involves myriad puzzles and potential complications that, so far, no gene therapy efforts have been able to surmount. “It’s the kind of thing that looks great on the drawing board,” says Erik Sontheimer, a CRISPR researcher at Northwestern University. “But in reality, it’s going to be a tough nut to crack, because drug delivery is going to be a real challenge.”
Most scientists agree that any practical CRISPR-based therapies are still far in the future, but some are already researching possible solutions to the drug delivery challenge, including nanoparticle delivery, and “phagemids”—hybrids that encapsulate bacterial DNA, replete with antibiotic resistance genes, inside a phage virus capable of invading bacteria. In theory at least, if you had a phagemid that contained a CRISPR sequence with resistance genes, you could spray it on various surfaces where bacteria congregate. The bacteria would take up the phagemids, and incorporate the DNA contained therein. This would prevent them from acquiring or expressing those resistance genes. But while these things work pretty well in the lab, making them work in a hospital is a different story. For one thing, FDA approval of live phage spray is expected to be hugely problematic.
Still, CRISPR remains immensely promising. In the past few years there has been an explosion of research into this curious code and its mysteries. “When we held the first conference, back in 2007, there were so few CRISPR studies, I joked that you could read the entire literature in a day,” says Barrangou. “Now, there are literally hundreds of publications out there.”
And even if some potential CRISPR uses sound far-fetched, they shouldn’t be disregarded, Marraffini says. “There are many things we have today, that seemed like science fiction just a few decades ago,” he observes. “Including antibiotics.”
Jeneen Interlandi is a science writer based in New York. She was a 2013 Nieman Fellow and writes for The New York Times Magazine and Scientific American.