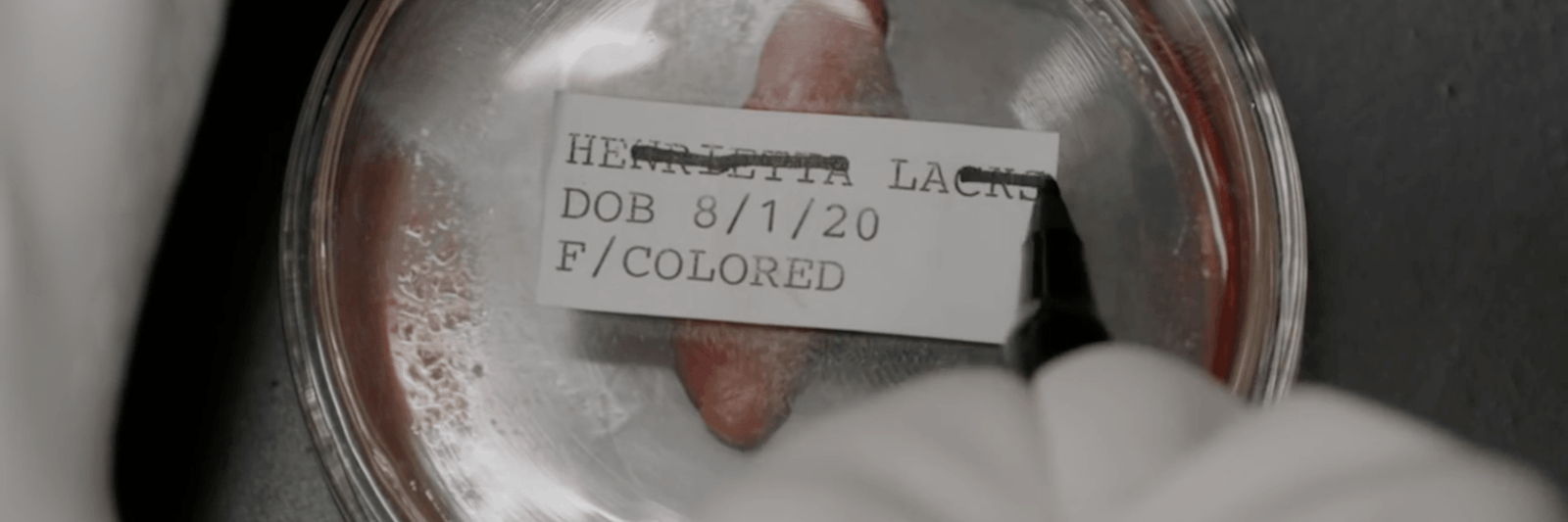
When HBO released its television film drama The Immortal Life of Henrietta Lacks starring Oprah Winfrey, earlier this year, it may have reawakened some Americans to a dark chapter of scientific research. Based on investigative journalist Rebecca Skloot’s book of the same name, it chronicles the endeavors of the author Deborah Lacks to unearth the medical history of Deborah’s mother, Henrietta, a poor black woman diagnosed with cervical cancer. In 1951, after visiting her doctor, George Grey, Lacks could not have fathomed that her cancer cells would go on to make life-saving discoveries like the polio vaccine, among other things—all without her consent.
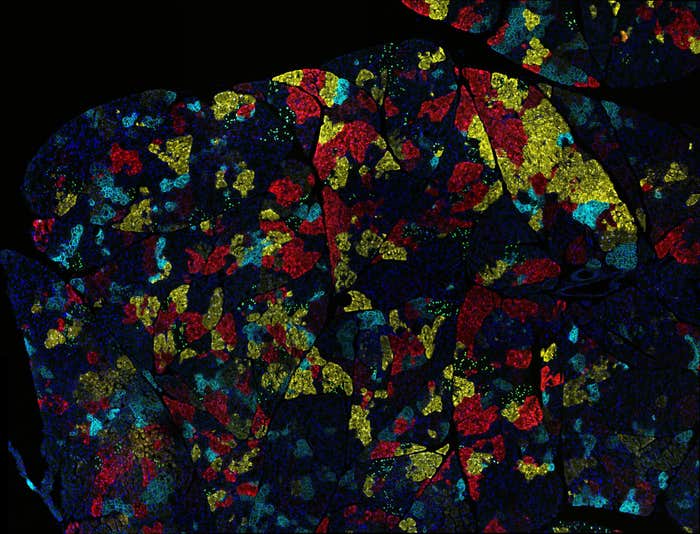
What made these cells so game-changing was their durability. At the time, it was normal for cells to die after being cultured for a few days. But Lacks’ cells didn’t die. They reproduced and survived, becoming not just the first “immortal” cell line, named HeLa, but a boon to medical and biological researchers. By the time her book was published in 2010, Skloot wrote that “more than 60,000 scientific articles had been published about research done on HeLa, and that number was increasing steadily at a rate of more than 300 papers each month.” This required scientists to grow around 20 tons worth of her cells, generating billions of dollars for the biomedical industry. Lacks’ family still hasn’t seen a penny of the profits.
In fact, a 1991 rule was supposed to protect patients and research subjects from this happening. Officials then established the Federal Policy for the Protection of Human Subjects, better known as “the Common Rule,” a broad set of ethical guidelines for federally funded research on human subjects. A number of federal agencies including the Departments of Agriculture and Energy, as well as the Department of Health and Human Services, adopted it. But despite major overhauls and advances, like the digitization of medical health records and privacy concerns related to advanced genomics capacities like large-scale, data-generation platforms, the rule hasn’t changed. It wasn’t until the publication of Skloot’s book that the Department of Health and Human Services, along with other agencies, considered updating it.
“Those specimens are invaluable to what we do.”
Andy Shuman, a surgical oncologist and clinical ethicist at the University of Michigan Medicine, said that after two decades, the Common Rule was in serious need of revisions. Shuman summarized and analyzed the proposed changes to the Common Rule in a co-authored paper, published online in April in the Journal of Clinical Oncology. One significant update to the Common Rule, in light of Lacks’ case, is to require research agencies implementing the rule to consider, every four years, what an “identifiable biospecimen”—like the HeLa cancer cell line—means, since it’s expected that innovations will open up new ways of identifying who a biospecimen belongs to. New tech could render previously nonidentified biospecimens—which don’t require consent to use—identifiable.
The revisions were written into the Common Rule in January, 2017, just a few days before the inauguration of President Trump. In the Journal of Clinical Oncology, the authors note the revisions, or “Final Rule,” are not slated to take effect until January, 2018, and express concern the Trump administration could revoke the changes. “The presidential administration, as well as Congress, have promised significant changes and reconsideration, if not blanket rejection, of many of the preceding administration’s executive actions,” they write, adding, “The current leadership’s promises to undo or perhaps dismantle the culmination of almost 6 years of thoughtful consensus will only lead to unsettlement, exasperation, and confusion that would undo a carefully crafted bipartisan effort.”
Nautilus spoke with Shuman to discuss how the Common Rule protects patients, how it defines a “human subject,” and whether it’ll become politicized like other areas of science.
How has Lacks’ story shaped the Common Rule’s update?
One of the biggest problems with Henrietta Lacks’ story, besides her lack of consent, is that the cell line itself was actually named in a way that was identifiable. Anything that’s identifiable requires consent. One of the main changes was that the Common Rule does not apply to deidentified specimens. And that clarifies the position that biospecimens that are not identifiable with patient identifiers are fair game for research. That was a big sigh of relief for the research community, specifically the cancer research community, because those specimens are invaluable to what we do.
Are you worried that the White House might undo the Final Rule?
The most important point to make is that oncology research is not partisan. It’s not a matter of blue versus red—it’s us versus cancer. The Common Rule revisions reflect a thoughtful bipartisan effort and should be viewed as such. Many of the concerns regarding National Institutes of Health funding are scary for cancer researchers, and the Precision Medicine Initiative as well as the Cancer Moonshot are simply not tenable without federal support. And medical research is one of the most valuable uses of our tax dollars. The March for Science illustrated this point clearly, and without a need for political grandstanding or partisanship—that medical research, and cancer research specifically, is a fundamental need and one from which all of us stand to benefit.
Why is the Common Rule being revised now?
The advent of genetics, as well as other technological and medical innovations, have changed the playground from where we were in 1991. In the last six years, there’s been public debate to better understand how we should evolve the regulatory framework for human subjects research. There really needed to be an update that reflected how research is actually done and recognizing both historical transgressions as well as an evolution in how much the public wants to be engaged in this in a way that is really designed to protect human subjects, but also to empower the discoveries that the research is designed to achieve.
“The vast majority of ethical transgressions have involved the tragic treatment of human subjects as something less than human.”
What is a “human subject” exactly?
The proposed definition of a human subject, which preceded the Common Rule, questioned whether or not de-identified specimens would require consent and could be studied in an ethically defensible manner associated with minimal risk. The fact that de-identified specimens are not considered a “human subject” is being heralded among the scientific community because it’s going to allow the ongoing use of the specimens. Now, what is quite interesting is the new Final Rule is now required to consider what an “identifiable biospecimen” means every four years and to discuss how new technologies may create identifiable private information from otherwise non-identified specimens, how will the future of genetics and genomics create a situation in which we will be able to identify something purely by the genetics.
What harm can come to patient if their biospecimens are identifiable?
The main components of ethical research are informed consent, and protection of privacy, and protection from harm. With biospecimens work the harms that can potentially occur are the dissemination of information and/or privacy breaches. And potentially taking advantage of vulnerable populations of people, specifically those who have cancer or with other life-threatening diseases. We, as a field, have accepted that when we have biospecimens that are identifiable, patients need to consent for their use, and need to understand what potential harms may occur, which includes privacy breaches, as well as the fact that this information may or may not be shared with other parties. The other complicated part is recognizing that future research may not be anticipated right now. And when a specimen sits in a freezer for decades, the way it may be of value down the road may be different from what anyone can comprehend at the time of the biopsy or the resection.
Could these revisions impede, and possibly hurt, scientific research?
Sure, one of the major tensions in research ethics is the tension between facilitating meaningful research and protecting human subjects. The two need not be mutually exclusive. In general, the protection of human subjects will supersede the ability to do research that would otherwise be considered ethically problematic. However, even stakeholders, including potential and current patients recognize that the value that research offers in certain cases, will justify a certain amount of potential harm, but the research community has suffered many transgressions over history in a way that has taught us that transparency and protecting the supremacy of human subject dignity and intrinsic rights is also critical. That tension and that balance is something that researchers and those who evaluate these studies will constantly weigh against each other.
Is one of the big issues that you don’t want these patients to become giant lab rats?
When you ask anyone whether or not [stakeholders] want to be involved in decision making, and consent to a specimen’s use, the vast majority will say yes. Many actually prioritize the science and discoveries over involvement in the informed consent process, specifically when there was no particular harm that is identifiable. One of the main changes was that the Common Rule does not apply to de-identified specimens—biospecimens that are not identifiable with patient identifiers are fair game for research. That was a big sigh of relief for the cancer research community because those specimens are invaluable to what we do.
The hardest goal here is to ensure research is not inappropriately handcuffed by regulatory requirements, but similarly that human subjects’ rights are not ignored or devalued purely in the pursuit of science. The vast majority of ethical transgressions have involved the tragic treatment of human subjects as something less than human, and not privy to the rights and dignity that they deserve. A granular example for transgression in cancer research is Chester Southam. [He] led a clinical research trial without informed consent, in which he injected cells into patients with cancer as well as some without cancer to determine whether those would lead their immune system to fight disease. Those experiments were conducted without consent.
How much are patients concerned that their biospecimens will help researchers turn a profit?
It is absolutely true that there is potentially a great deal of money to be made. One of the things that our group has studied at Michigan Medicine is that patients are much more interested in understanding how research involving either them or their specimens will potentially lead to profit. We know that the vast majority of individuals want to know whether or not that is possible. From a practical standpoint, it is very rare for one specific specimen to generate any significant profit. However it’s not impossible. What is important to recognize is that researchers are transparent about their conflicts of interest and their potential for gain, but also honestly recognize that most of the time the research itself is going to cost more than any potential profit. With that said, I think that the public and all stakeholders deserve transparency in understanding how individuals as well as industry may benefit from their involvement.
Image credit: HBO / YouTube