This article from our 2013 issue, “In Transit,” offers a timely look at how an animal virus from one place can infect people across the world.
Sometime in 2004, a pig was trucked with a herd of others to Sheung Shui Slaughterhouse, Hong Kong’s largest abattoir. It could have been shipped from any number of farms in China. The pig was penned in cramped conditions and later shoved onto a conveyor line. When it reached the end of the line it was electrocuted with a jolt to the head. A worker slit its throat. Before its carcass was hoisted up on a chain, scalded, and cleaned, scientists swabbed the pig’s mouth as part of a flu-monitoring program, run by Hong Kong University. The pig carried a seemingly harmless strain of influenza. The strain was genetically sequenced, baptized Sw/HK/915/04, entered into a database, and forgotten.
Five years later a flu epidemic, which originated in pigs, raced around the globe through air travel, leaving a trail of nearly 300,000 people dead from the United States to Brazil, China to New Zealand, South Africa to Finland. Scientists determined the outbreak began in Mexico, not far from a huge pig breeding farm. Poring over databases, looking for clues to the makeup of the killer virus, scientists discovered that Sw/HK/915/04, the influenza strain of the Hong Kong pig, shared seven of its eight genes with the strain of 2009.
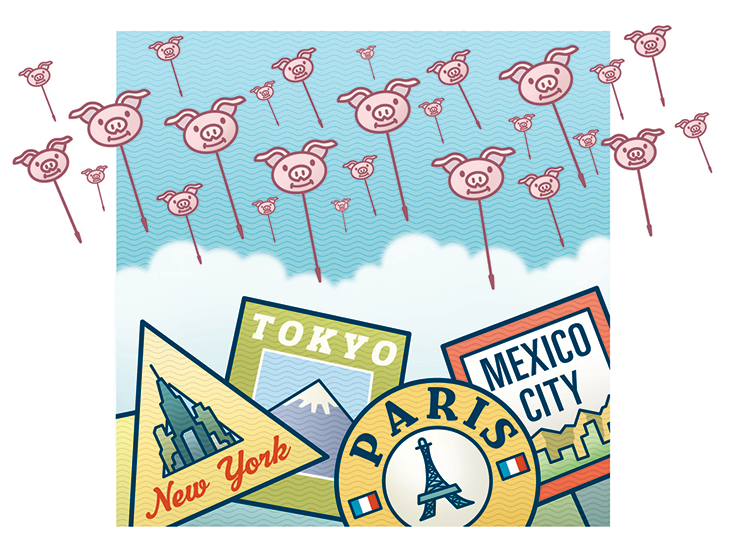
The 2009 flu epidemic stripped back the veil on the dangers of our interconnected world.
The shared genes suggest to scientists that the 2009 virus may have evolved by mixing genomic segments of viral strains in pigs from around the world. Global shipments of pigs are seldom tracked and researchers did not establish a direct link between the infected Hong Kong pig and the 2009 outbreak in Mexico. “We don’t really have information about pig viruses in Mexico,” says Gavin Smith, an evolutionary biologist based at Duke-NUS Graduate Medical School, part of the National University of Singapore, and lead author of a Nature paper on the origins of the 2009 epidemic. “It was probably generated locally but genetic components could have come from Asia.”
Smith echoes what international health officials and scientists say may be the most worrisome aspect of viruses today: the ease and speed with which some travel across the globe. The 2009 flu epidemic, they say, stripped back the veil on the dangers of our interconnected world. “Pathogens evolve and spread in a world where our mobility is very different than it was 50 to 100 years ago,” says Dirk Brockmann, a theoretical physicist at Northwestern University, who studies the spread of infectious diseases, including the 2009 virus, classified as H1N1. “When a pathogen emerges that has human transmissibility, like the H1N1 virus, that is a massive risk.”
Today factory swine farms and slaughterhouses provide pathogens an orgy of evolutionary opportunities. Pigs, it turns out, are veritable incubators of Influenza A, the common affliction that causes fevers, lethargy, snotty outbursts, and at least tens of thousands of deaths every year. The Spanish Flu of 1918 and 1919, an influenza that killed up to 50 million people, evolved inside a pig and jumped to humans. The H1N1 virus of 2009 was a subtype of Influenza A.
Influenza A spreads from animals to humans, and human to human, through touch, breath, or blood. (Cooking meat kills the virus.) Migratory ducks and other waterfowl were the original carriers of Influenza A, sharing ancient strains of the virus among themselves. It is relatively difficult, though, for a person to catch a strain of bird flu, and vice versa. But pigs can be go-betweens. They can contract Influenza A from birds, humans, and other pigs.
Influenza A generally contains eight gene segments. It quickly evolves when different strains exchange gene segments, giving rise to new mutant varieties. “As the infected cell is replicating,” explains Smith of Duke-NUS, “the individual gene segments can package one gene from one virus and seven genes from the other virus. Or, really, any other combination.”
Most mutant strains are failures. But sometimes a strain is produced through genetic recombination and reassortment that’s more “fit” in the Darwinian sense than either of its ancestors. The viruses that dwelled inside the 2004 Hong Kong pig and its deadly cousin in Mexico were triple-recombinant. They assembled genes that originated from strains of human, pig, and bird flu together into a single strain.
Factory slaughterhouses like Sheung Shui in Hong Kong, where pigs are penned together before they’re killed, exacerbate the problem. Sheung Shui was built in 1999 to consolidate operations of three smaller Hong Kong abattoirs, save on land, and improve efficiency. Pigs are shipped there from nine provinces in China to meet a growing demand for meat in increasingly affluent Asia. Sheung Shui slaughters about 5,000 pigs a day.
In the past, when pigs were confined to their respective farms, explains Malik Peiris, a professor of virology at the University of Hong Kong, flu strains festered but remained in relative isolation. Now, pigs from different regions are transported together and share saliva, air, and germs. Thrown together, they create a viral hub. “You can’t keep the pigs isolated,” says Peiris, who carries out surveillance for influenza viruses at the Sheung Shui Slaughterhouse. “There are opportunities for transmission from one set of pigs to another.”
On an international scale, Peiris adds, “The dogma was always that pig viruses don’t move around. I mean, pigs don’t fly.” But, he says, his research has “clearly showed movement of viruses from North America to China, from Europe to China.” He says breeder pigs, which countries exchange, fuel the spread of viruses.
“Movement of infected animals does increase the risk of transmission,” says Smith. “The danger is that you have different types of viruses in different pig populations. And the mixing of different strains increases the diversity of viruses.”
The pig alone, though, isn’t responsible for epidemics. After all, a virus can infect a pig without causing anything more serious than sniffles and a touch of fever. In fact, because viruses don’t usually kill adult pigs, many farmers don’t bother to vaccinate them. “It would be a waste of money because they don’t have major economic losses, so there’s not enough to justify vaccination,” says Shirley Chuk, a senior veterinary officer in the Hong Kong government. The best defense is to prevent the flu from jumping from pigs to humans. “With farmers, we always advise them to observe personal hygiene,” Chuk says.
But of course it’s never enough. Scientists couldn’t pinpoint how H1N1 jumped from swine to humans in 2009. But they do know that once it did, modern air travel became a viral expressway.
Now, pigs from different regions are transported together and share saliva, air, and germs. Thrown together, they create a viral hub.
The problem begins with airports, says Christos Nicolaides, a doctoral candidate at the Massachusetts Institute of Technology, who studies dynamic processes within complex networks. A main factor is an airport’s “traffic field,” which describes an airport’s interconnectedness with other airports. Predictably, New York and Los Angeles are “influential spreaders.” But so, for instance, is Hawaii, which has 30 percent less air traffic than New York. Positioned in the middle of the Pacific Ocean, Hawaii is linked with many of the world’s major hubs. Once a sick person shows up in a Hawaiian waiting lounge, coughing over their fellow travelers, the disease can quickly radiate out to the world’s other major air hubs, and beyond.
Focusing on the interconnectedness among cities based on air traffic, rather than their distance apart, is a key to understanding how an epidemic metastasizes, says Brockmann, the Northwestern physicist who has studied the 2009 epidemic. To understand modern pandemics, he says, we need to think of the world in terms of “effective distance.”
In a conventional sense, London and New York are 3,500 miles apart, while London and Edinburgh are about 400 miles apart. But when you rely on an intuitive sense of how the cities are connected, taking into account the air traffic between them, London and New York are effectively next-door neighbors, while London and Edinburgh are distant cousins.
Pandemics, Brockmann has shown, rapidly spread across the globe through mobility networks. In April 2009, when the Centers for Disease Control and Prevention issued a public alert about the H1N1 virus, Brockmann applied his methods to the epidemic. Over the course of two weeks after the alert, he projected a worst-case scenario (in which no steps to contain the disease were taken) of where H1N1 would spread in the U.S. Pinpointing Mexico City as the disease epicenter, and based on air-traffic data and demographics, he projected that 90,000 flu cases would congregate in five regions or “hot spots”: Southern California, Dallas, the Northeast, Chicago, and Miami. Matched against final CDC data, which showed both the number of confirmed and suspected cases across the nation in the first few weeks of the outbreak, Brockmann’s projections were remarkably accurate. Only Miami turned out to be a miscalculation, though the numbers of infections in that area did grow exponentially over the summer of 2009.
Clearly, mathematical projections about how pandemics spread are valuable. If a disease epicenter is unknown, Brockmann says, he can perform a type of reverse engineering with his computer simulations, starting with regions where infections have been reported. “We can then identify where the epicenter is, and we can predict when a disease is going to arrive somewhere,” he says. Unfortunately, mathematical projections can’t stop a pandemic.
In 2011, an international team of computational epidemiologists at the Institute for Scientific Interchange in Italy, Northeastern University of Boston, and the French National Institute of Health and Medical Research, analyzed the global spread of the 2009 pandemic. They examined travel bans to Mexico instituted by countries around the world, airport screenings for potentially infected passengers, and advisories against traveling to Mexico. A month after the international alert, they determined there was a 40 percent drop of international air flow in and out of Mexico City. That 40 percent decrease, however, only “led to an average delay in the arrival of the infection in other countries (i.e., the first imported case) of less than three days.” The scientists then projected what would happen if 90 percent of air travel to and from Mexico had been restricted, and the results were not much more hopeful—a 90 percent restriction would have delayed the spread by, at most, 20 days.
In their report, “Human Mobility Networks, Travel Restrictions, and the Global Spread of 2009 H1N1 Pandemic,” published in the journal PLOS One, the scientists offered a dire conclusion: “It is unlikely that given the ever-increasing mobility of people, travel restrictions could be used effectively in a future pandemic event.”
The grim outlook for halting a future pandemic is shared by computational scientists, virologists, and microbiologists. Pandemics, they say, are the dark side of global mobility. Smith, an exacting scientist with a dry delivery, notes there is one “drastic option.” “The best way to stop the spread of infection is to stop travel,” he says.
John Upton is the Partnerships Journalism Editor at Climate Central.






























